The reversed halo sign (also known as the atoll sign) is a radiological finding characterized by a central area of ground-glass opacity surrounded by a ring or crescent of denser consolidation. This pattern is most commonly observed on CT scans of the chest and indicates a variety of underlying pulmonary pathologies, typically involving inflammatory, infectious, or vascular processes.
Etymology
- Derived from the term “halo” (a ring or circle of light) with “reversed” indicating the opposite pattern.
- “Atoll” refers to a ring-shaped coral reef or island, symbolizing the radiologic appearance.
AKA
- Atoll Sign
What is it?
- The reversed halo sign is a radiologic finding characterized by a central ground-glass opacity surrounded by a ring-like area of denser consolidation.
- It is typically associated with specific infectious, inflammatory, or neoplastic processes.
Characterized by
- A ring-like consolidation encircling an area of ground-glass opacity.
- Central opacity is less dense than the surrounding ring.
- Most often visualized on CT imaging.
Anatomically affecting
- The lung parenchyma, often localized to regions of inflammation or infection.
Pathophysiology
- Reflects underlying pathological processes, including:
- Central ground-glass opacity: Represents alveolar inflammation, hemorrhage, or edema.
- Peripheral ring consolidation: Represents granulomatous inflammation, fibrosis, or cellular infiltration.
How does it appear on each relevant imaging modality?
Principles
- Parts: Ground-glass center surrounded by a dense ring of consolidation.
- Size: Varies with the underlying lesion, generally measured in centimeters.
- Shape: Circular or oval, with sharp or irregular edges.
- Position: May occur in any part of the lung but is commonly seen in peripheral regions.
- Character: Contrast between a less dense center and more dense outer ring.
- Time: Evolution depends on the underlying disease process (acute or chronic).
CXR
- Rarely visualized due to its subtle nature.
- May appear as a faint ring-like opacity or subtle consolidation.
CT
- Key Modality: High-resolution CT (HRCT) is the gold standard for identifying this finding.
- Central ground-glass opacity surrounded by a dense ring of consolidation.
- Sharp differentiation between the inner ground-glass region and the outer consolidation.
- May show associated features like nodules, cavitation, or air bronchograms depending on the etiology.
MRI
- Limited utility for this finding.
- Can demonstrate central ground-glass opacities and peripheral ring consolidation on T2-weighted images.
PET-CT
- Increased metabolic activity may be observed in the surrounding consolidation.
- Central ground-glass opacity may show variable activity depending on the underlying etiology.
Other Modalities
- Ultrasound: Not applicable.
- Fluoroscopy: Rarely used.
Differential Diagnosis
- Infectious Causes:
- Fungal infections (e.g., mucormycosis, aspergillosis).
- Tuberculosis.
- Inflammatory Causes:
- Cryptogenic organizing pneumonia (COP).
- Granulomatosis with polyangiitis (Wegener’s granulomatosis).
- Neoplastic Causes:
- Lung adenocarcinoma with lepidic growth.
- Other Causes:
- Sarcoidosis.
- Pulmonary infarction.
Recommendations
- Further imaging: Contrast-enhanced CT to assess lesion vascularity and adjacent structures.
- Laboratory correlation:
- Fungal cultures, blood work, and serological tests for infectious etiologies.
- Autoimmune markers for vasculitis or inflammatory conditions.
- Biopsy: Consider for definitive diagnosis, particularly in suspected malignancy or granulomatous disease.
Key Points and Pearls
- The reversed halo sign is not disease-specific but is most commonly associated with cryptogenic organizing pneumonia (COP).
- It requires clinical and laboratory correlation to narrow down the differential diagnosis.
- Early recognition on imaging, particularly CT, can guide timely and appropriate intervention.
- Its presence in fungal infections (e.g., mucormycosis) warrants urgent treatment due to potential rapid progression.

Reconstruction of an atoll which is an is a ring-shaped island, including a coral rim that encircles a lagoon. There may be coral islands on the rim. Atolls are located in warm tropical or subtropical parts of the oceans and seas where corals can develop. Most of the approximately 440 atolls in the world are in the Pacific Ocean.
Artistic rendering by ChatGPT
and Wikipedia
Ashley Davidoff MD TheCommonVein.net
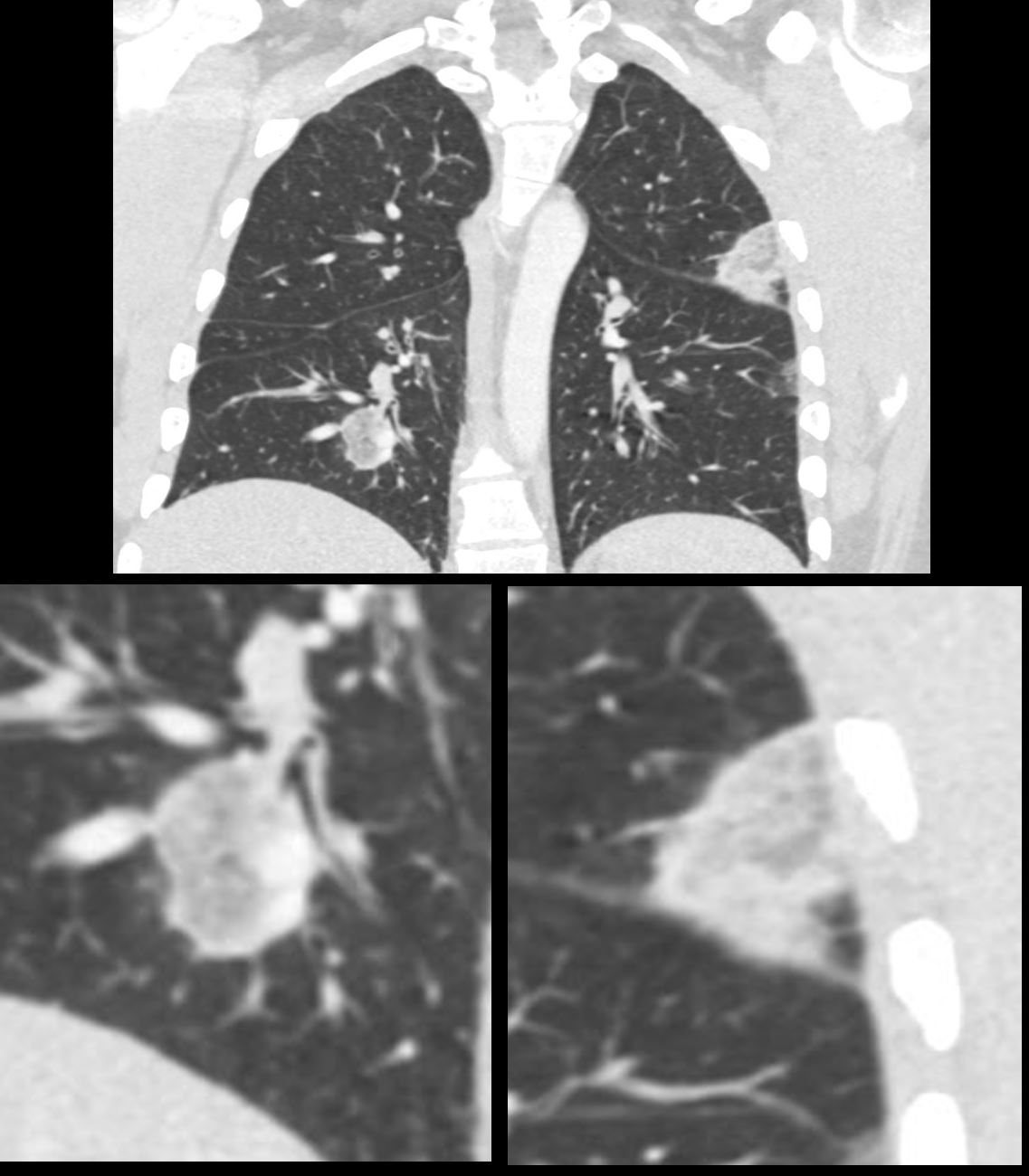
The nodule consists of a peripheral dense border surrounding a ground glass opacity, similar in appearance to an atoll
Ashley Davidoff MD TheCommonVein.net 139137c
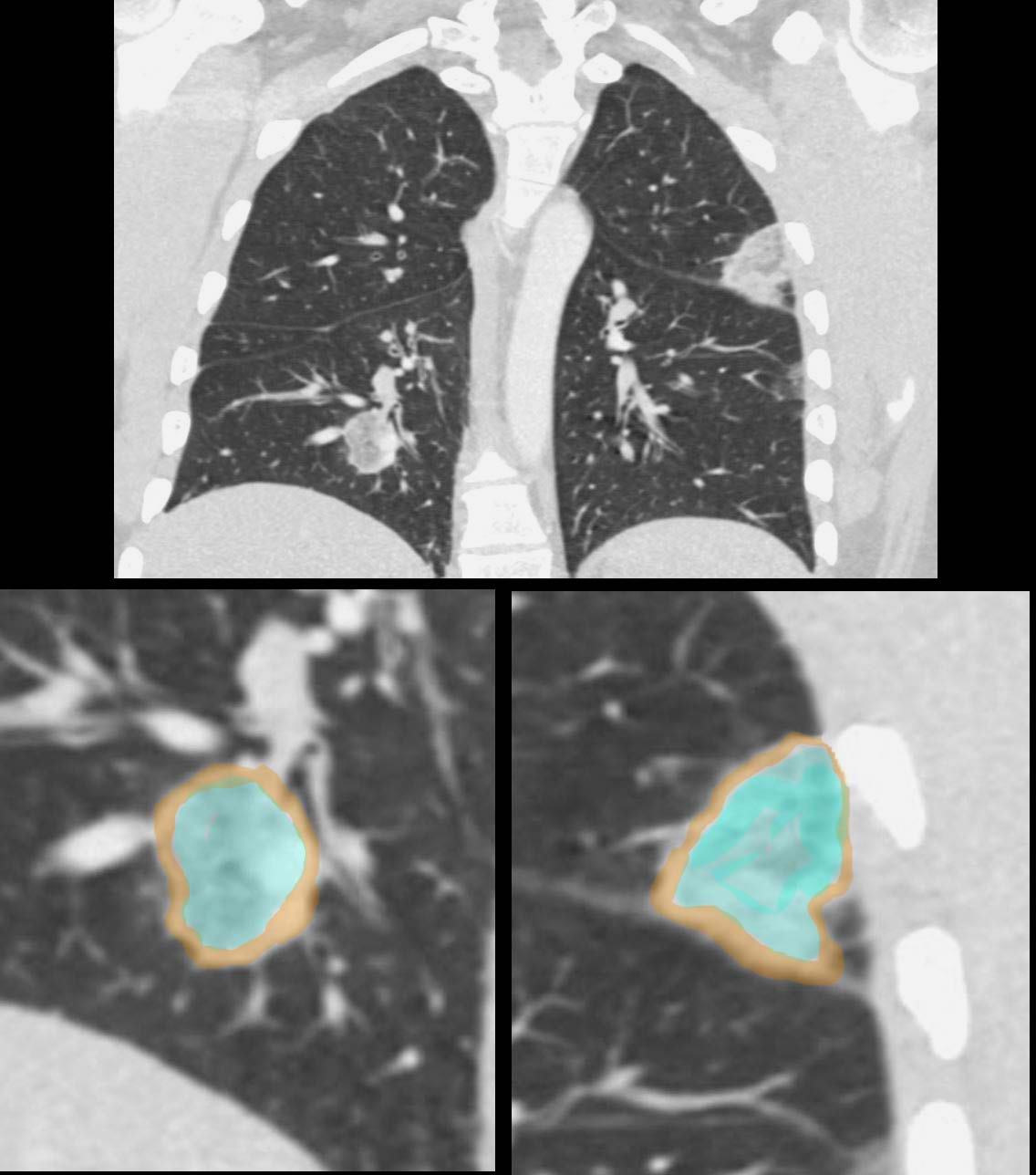
The nodule consists of a peripheral dense border (overlaid in brown) surrounding a ground glass opacity overlaid in turquoise)
similar in appearance to an atoll
Ashley Davidoff MD TheCommonVein.net 139137cL
It is associated with various lung conditions, most notably
organizing pneumonia (OP), although it can also be seen in other
diseases such as pulmonary infarction, granulomatosis with
polyangiitis, and fungal infections.
Lung biopsy may be carried out
to confirm the underlying cause.
Laboratory tests and cultures may
also be used if infection or autoimmune disease is suspected.
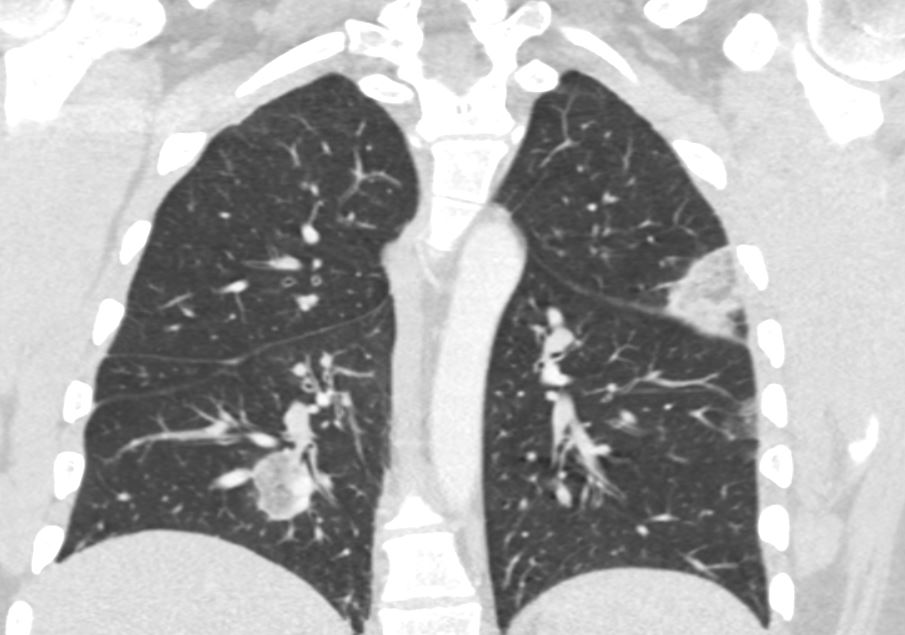
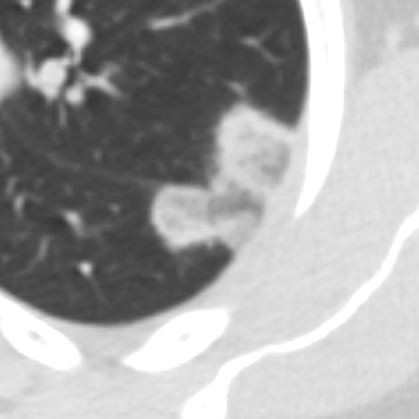
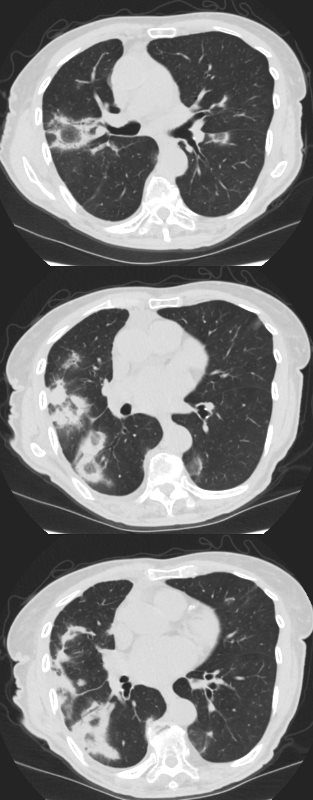
Hemorrhagic PE with with Reversed Halo Sign
32 year old male presents with acute PE and reversed halo sign indicative most likely of a hemorrhagic pulmonary infarction
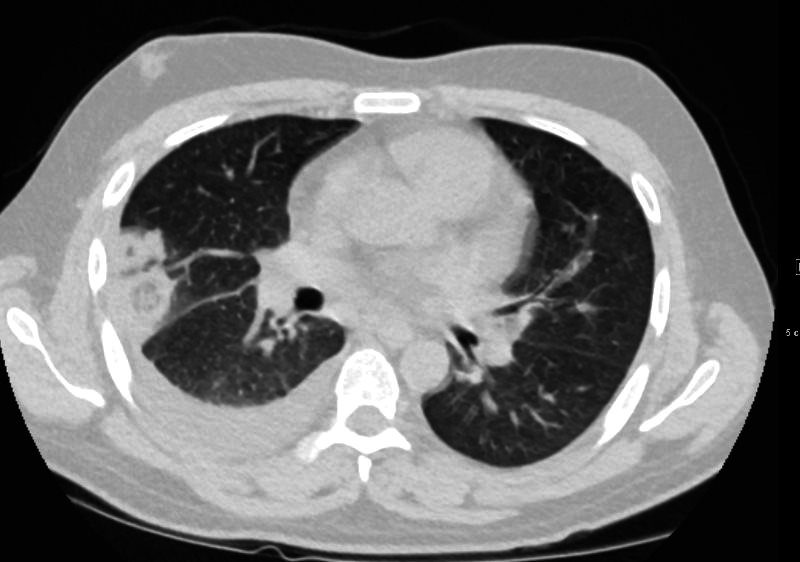
32 year old male presents with acute PE and reversed halo sign indicative most likely of a hemorrhagic pulmonary infarction
Ashley Davidoff MD

32 year old male presents with acute PE and reversed halo sign indicative most likely of a hemorrhagic pulmonary infarction
Ashley Davidoff MD
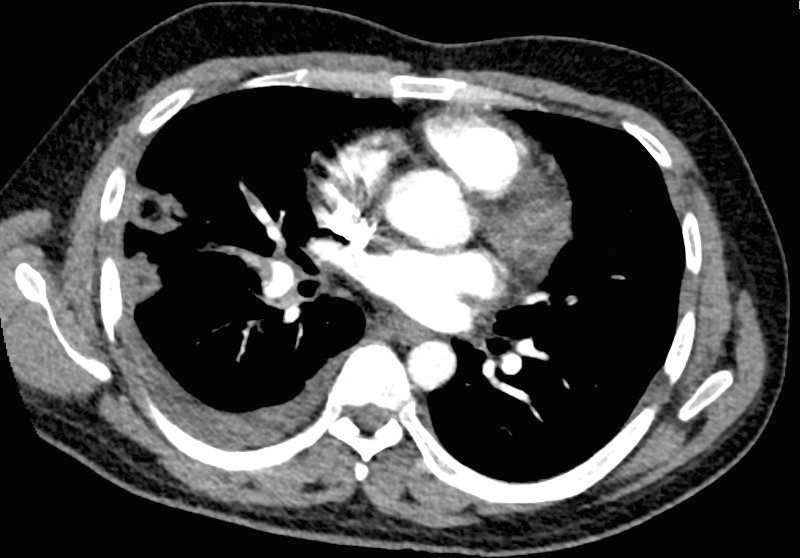
32 year old male presents with acute PE and reversed halo sign indicative most likely of a hemorrhagic pulmonary infarction
Ashley Davidoff MD
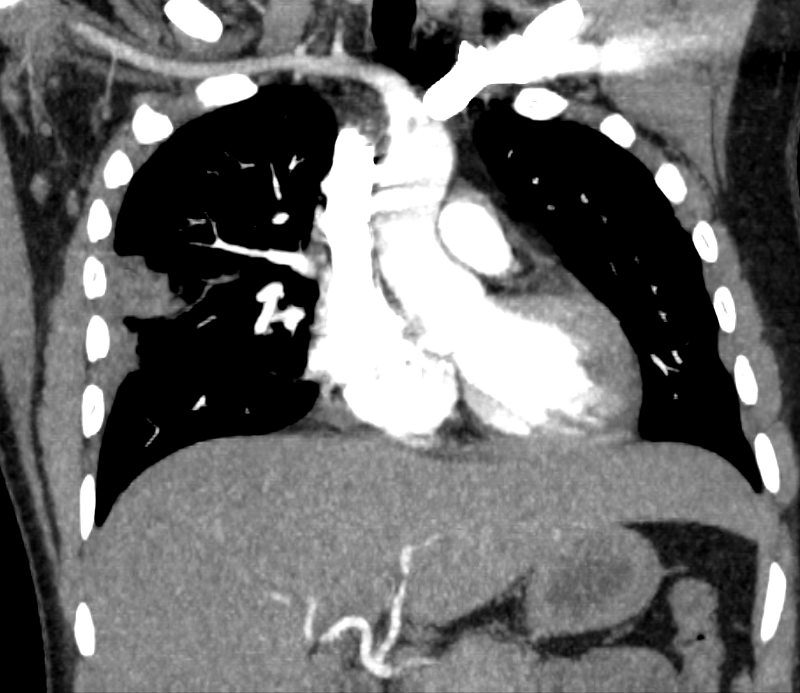
32 year old male presents with acute PE and reversed halo sign indicative most likely of a hemorrhagic pulmonary infarction
Ashley Davidoff MD
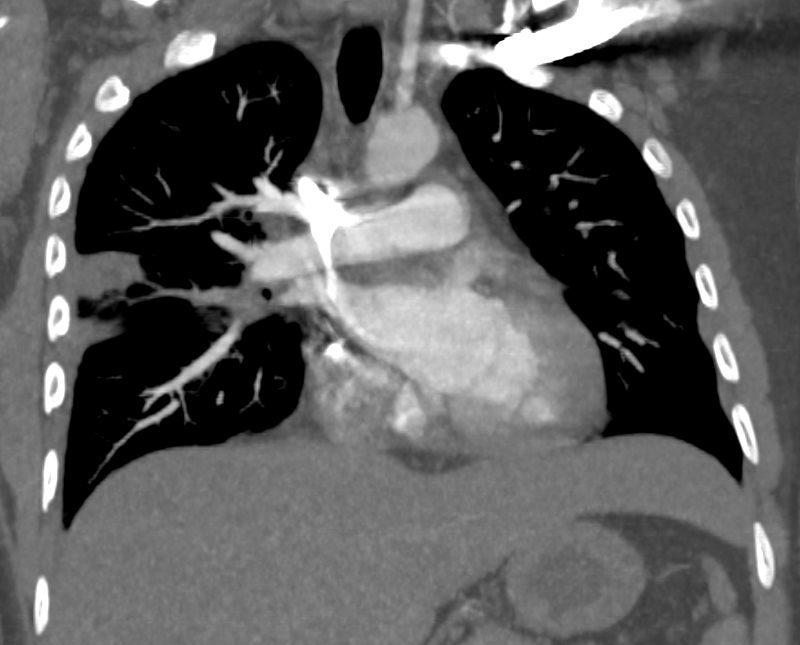
32 year old male presents with acute PE and reversed halo sign indicative most likely of a hemorrhagic pulmonary infarction
Ashley Davidoff MD
Reversed Halo Sign Related to Immunotherapy for Adenoca of the Lung
87-year-old female with stage IV adenocarcinoma s/p immunotherapy
In the initial scans there are prominent lesions demonstrating the reversed halo sign likely as a result of the therapy
Subsequent imaging (2 CT scans) shows progressive resolution of the multicentric changes
87-year-old female with stage IV adenocarcinoma s/p immunotherapy
In the initial scans there are prominent lesions demonstrating the reversed halo sign likely as a result of the therapy
Subsequent imaging (2 CT scans) shows progressive resolution of the multicentric changes
Ashley Davidoff MD 131478.8
Follow Up 2 Months Later

87-year-old female with stage IV adenocarcinoma s/p immunotherapy
In the initial scans there are prominent lesions demonstrating the reversed halo sign likely as a result of the therapy
Subsequent imaging (2 CT scans) shows progressive resolution of the multicentric changes
Ashley Davidoff MD
Follow Up 6 Months Later
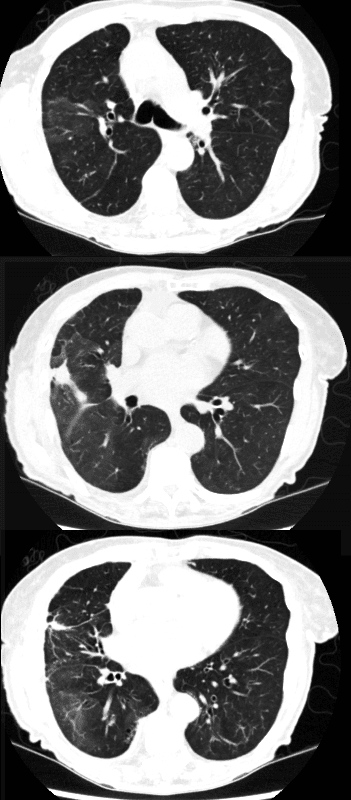
87-year-old female with stage IV adenocarcinoma s/p immunotherapy
In the initial scans there are prominent lesions demonstrating the reversed halo sign likely as a result of the therapy
Subsequent imaging (2 CT scans) shows progressive resolution of the multicentric changes
Ashley Davidoff MD
Young Man with Pleuritic Pain
Broad Differential Diagnosis

31 year old male with a history of DKA, brachial DVT and pleuritic pain presents for a CTPA to evaluate for pulmonary embolism. Findings show no acute PE’s, but he has multicentric, bilateral, peripheral based foci with reversed halo signs, (atoll sign). While chronic PE is on the differential diagnosis, the atoll sign is an unusual consequence of PE . Organizing pneumonia, fungal infections, – mucormycosis, aspergillosis, TB and chronic manifestations of a COVID infection are on the differential diagnosis
The nodule consists of a peripheral dense border surrounding a ground glass opacity, similar in appearance to an atoll
Ashley Davidoff MD TheCommonVein.net 139135
The concept of a halo has been widely used across cultures, often symbolizing divinity, protection, enlightenment, and guidance. Here are key ways it has been interpreted:
Halo in Cultural Symbolism
- Religious and Spiritual Contexts:
- In many religious traditions, the halo is depicted as a radiant circle surrounding the head of a deity, saint, or enlightened being.
- Christianity: Halos signify holiness and divine favor, often encircling Christ, Mary, and saints in religious art.
- Hinduism and Buddhism: Similar radiant circles, often called “aura” or “mandorla,” represent spiritual enlightenment or divine energy.
- Islamic Art: Halos are less common but sometimes appear in Persian or Mughal illustrations of prophets and religious leaders.
- Astronomical and Celestial Representation:
- Halos around celestial bodies like the moon or sun are interpreted as omens or signs of change in folklore and mythology.
- Lunar halos, for example, are linked to cycles of renewal and transition.
- Symbol of Authority and Protection:
- The halo conveys protection, with circular designs in armor or shields reflecting invincibility or a divine safeguard.
- It also signifies leadership and authority, seen in crowns or wreaths that mimic the halo’s circular form.
- Artistic and Cultural Depictions:
- Ancient Roman and Greek art used halos (or “nimbus”) to denote gods, emperors, or leaders.
- In the Renaissance, halos evolved into more subtle or symbolic forms in art, integrating light and shadow.
- Modern Symbolism:
- Halos in contemporary culture often represent purity, morality, or a guardian-like quality, as seen in literature, film, or graphic design.
- They are also used metaphorically in phrases like “halo effect,” indicating an overall positive perception based on a single favorable attribute.
-