Etymology
- Derived from the term small airways, referring to airways less than 2 mm in diameter, and disease, indicating pathological changes.
AKA
- Bronchiolitis
- Small airway obstruction
Definition
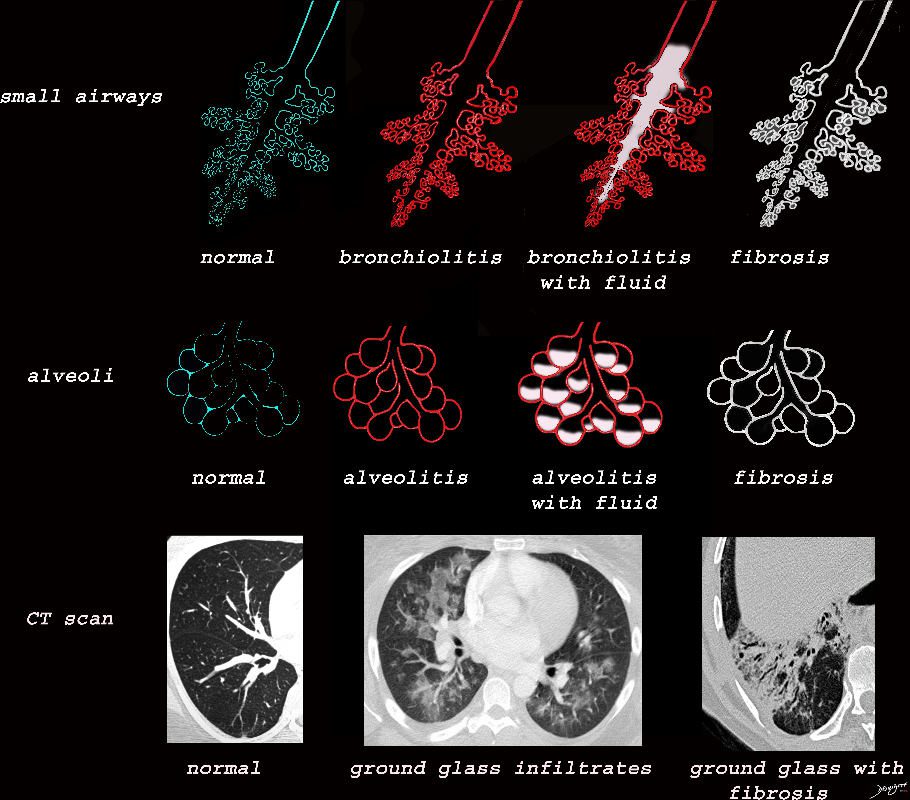
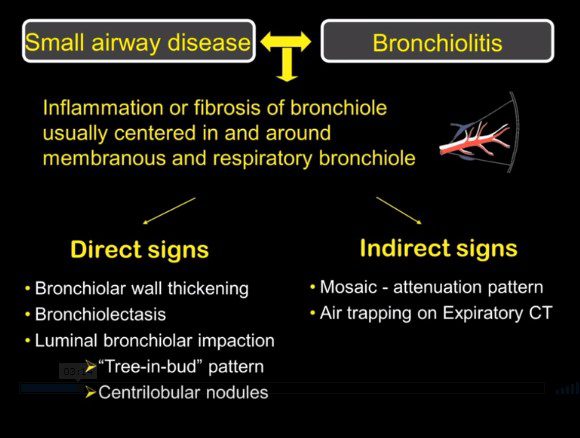
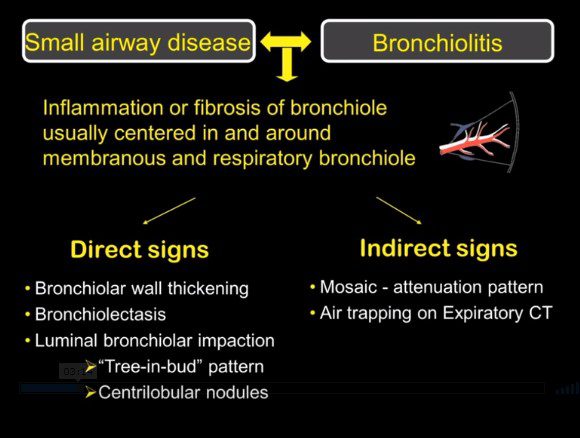
- What is it? Small airway disease encompasses a group of conditions affecting the bronchioles (airways <2 mm in diameter), characterized by inflammation, fibrosis, or obstruction that impairs airflow.
- Caused by:
- Inflammation: Chronic exposure to irritants (e.g., cigarette smoke, environmental pollutants).
- Infection: Viral or bacterial bronchiolitis.
- Autoimmune: Diseases like rheumatoid arthritis or sarcoidosis.
- Obstruction: Airway narrowing or collapse from fibrosis or external compression.
- Resulting in:
- Structural changes: Narrowing, obliteration, or dilation of small airways.
- Pathophysiology: Airflow limitation due to obstruction or loss of elastic recoil.
- Pathology: Chronic inflammation, peribronchiolar fibrosis, and mucus plugging.
- Diagnosis:
- Clinical: Symptoms include progressive dyspnea, wheezing, cough, or exercise intolerance.
- Radiology: Detectable on imaging, with findings such as mosaic attenuation or air trapping on expiratory CT.
- Labs: Typically non-specific; blood tests may show markers of systemic inflammation or autoimmune activity.
- Treatment: Management includes addressing underlying causes, smoking cessation, bronchodilators, anti-inflammatory therapies, and immunosuppressants when appropriate.
Radiology
- CXR
- Findings: May appear normal in early disease or show hyperinflation, peribronchial thickening, or areas of low density.
- Associated Findings: Subtle findings may include small opacities or signs of air trapping.
- CT
- Parts: Bronchioles and surrounding interstitium.
- Size: Affects airways <2 mm in diameter.
- Shape: Irregular or constricted bronchioles, often with thickened walls.
- Position: Typically diffuse but can be focal in certain diseases.
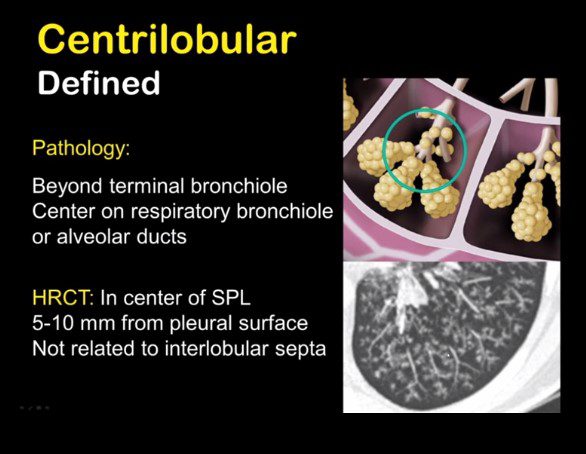
- Character: Mosaic attenuation, centrilobular nodules, and areas of air trapping on expiratory imaging.
- Time: Chronic or progressive changes in inflammatory or fibrotic diseases.
- Associated Findings: Bronchiectasis, mucus plugging, and hyperinflation.
- Other Imaging Modalities
- MRI may provide functional ventilation-perfusion data in research settings.
- Ventilation-perfusion scans can highlight ventilation defects in severe disease.
Key Points and Pearls
- Small airway disease is often subclinical in early stages and detected through imaging or pulmonary function tests (PFTs).
- PFTs typically demonstrate an obstructive pattern with decreased FEV1 and FEV1/FVC ratio.
- Mosaic attenuation on CT is a hallmark finding, particularly when paired with expiratory imaging.
- Early detection and intervention can prevent progression to advanced airflow limitation or chronic obstructive pulmonary disease (COPD).
- Smoking cessation and environmental control are critical in management.
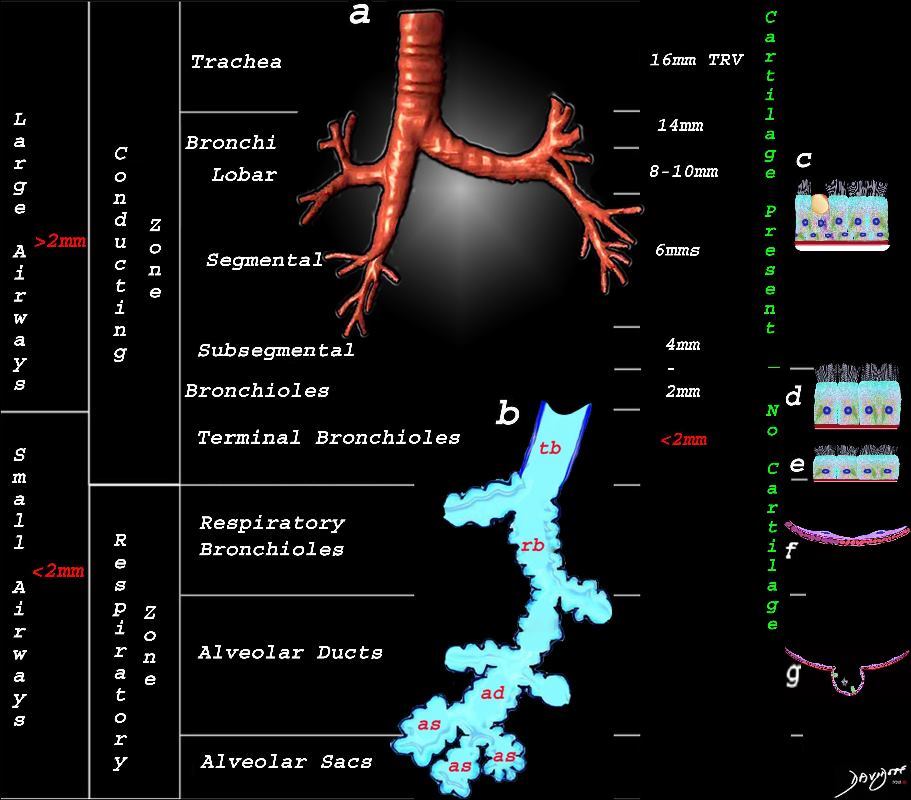
This image shows the division of the airways in the lungs classified as large airways and small airways.
Image (a) shows the airways starting in the trachea and continuing to the mainstem bronchi, lobar bronchi, segmental bronchi, and subsegmental bronchi.
Image b shows the structures that make up the small airways starting with the terminal bronchiole (tb) followed by the respiratory bronchiole (rb) alveolar duct, (ad) and alveolar sacs (as)
Image (c) shows the histologic makeup of the large airways that include a pseudostratified ciliated columnar epithelium with mucus secreting goblet cells a muscular layer (red) and a prominent cartilage layer (white) In the larger bronchioles (d) the epithelium remains as a pseudostratified, ciliated, columnar epithelium with prominent muscular layer (red). The columnar epithelium transitions to a stratified ciliated cuboidal epithelium by the terminal bronchiole s (f) both still with a muscular layer. The respiratory epithelium transitions from a cuboidal epithelium to a squamous epithelium (f) with alveoli and type I and II pneumocytes starting to branch (g)
Ashley Davidoff MD TheCommonVein.net lungs-0740nL
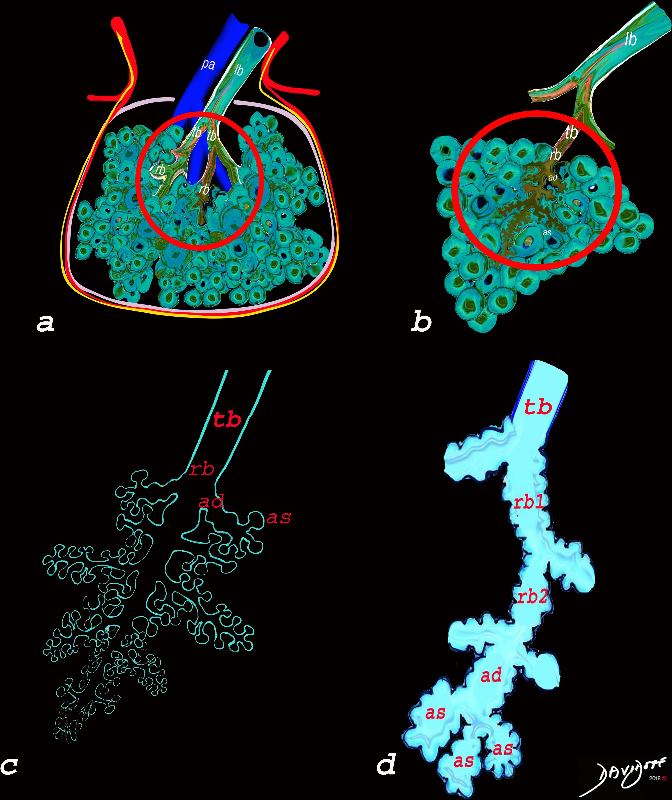
The diagram allows us to understand the the components and the position of the small airways starting in (a) which is a secondary lobule that is fed by a lobular bronchiole(lb) which enters into the secondary lobule and divides into terminal bronchioles (tb) which is the distal part of the conducting airways, and at a diameter of 2mm or less . It divides into the respiratory bronchiole (rb) a transitional airway which then advances into the alveolar ducts(ad) and alveolar sacs (as) Diseases isolated to the small airways do not affect the alveoli and hence there is peripheral sparing Ashley Davidoff MD TheCommonVein.net
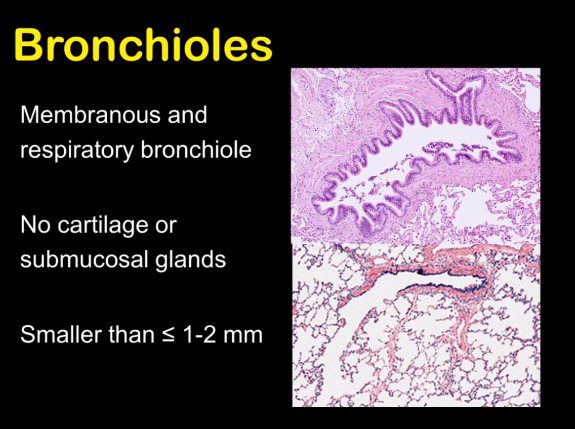
- Small Airways
-
- <2mm
- membranous bronchioles
- respiratory bronchiole
- lack cartilage
- lack submucosal glands
-
- Acinus
Terminal bronchiole Conducting Zone
Respiratory Bronchiole – Transitional Zone
Alveolar Ducts
Alveolar Sacs
Small Airways
The diagram allows us yo understand the the components and the position of the small airways starting in (a) which is a secondary lobule that is fed by a
- lobular bronchiole enters into the secondary lobule and
- divides into 3-12 terminal bronchioles (tb) which is the distal part of the conducting airways, and at a diameter of <than 2mm are considered the beginning of small airways. The terminal bronchiole divides into 2 respiratory bronchioles
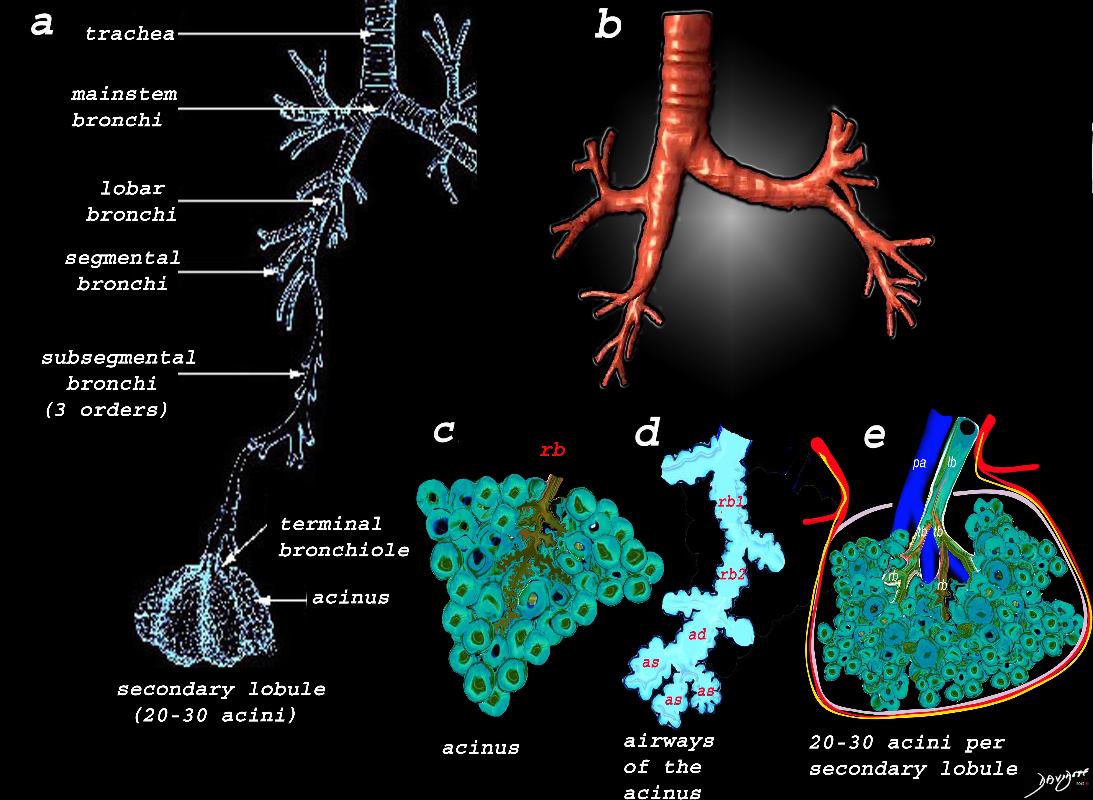
Image a shows the airways starting in the trachea and continuing to the mainstem bronchi, lobar bronchi, segmental bronchi, and subsegmental bronchi,. The subsegmental bronchi have 3 subsequent generations until the bronchiole is reached. The terminal bronchiole is the last of the transporting airways and is considered the most proximal small airway with a diameter of 2mm or less, and it gives rise to the respiratory bronchiole which is the feeding airway for the acinus . The acinus is the functional unit of the lung.
Image b is a 3D reconstruction of a CT scan showing the proximal airways from the trachea to the segmental airways.
Image c shows the structures that make up the acinus and the other parts of the small airways, starting with the respiratory bronchiole (rb) . The diagram in d, shows the detail of the small airways that participate in gas exchange, including the respiratory bronchiole, (rb) alveolar duct, (ad) and alveolar sac (as)
Image e shows the secondary lobule made from about 20-30 acini, arising from a single lobular bronchiole accompanied by a single pulmonary arteriole (pa).. Structure that surround and enclose the secondary lobule include the pulmonary venule, (red) lymphatics,(yellow) and a fibrous septum (pink).
Ashley Davidoff MD TheCommonVein.net
lungs-0739
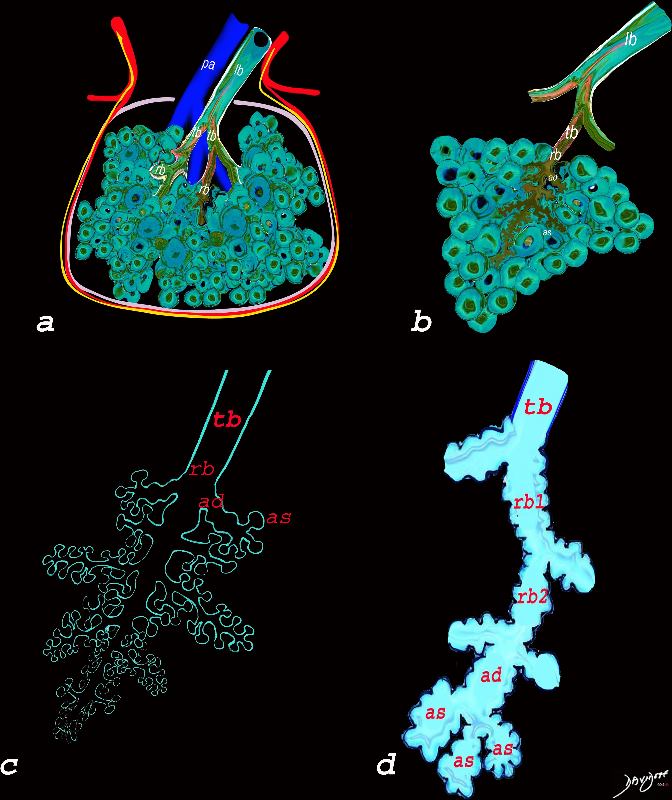
The diagram allows us to understand the the components and the position of the small airways starting in (a) which is a secondary lobule that is fed by a lobular bronchiole(lb) which enters into the secondary lobule and divides into terminal bronchioles (tb) which is the distal part of the conducting airways, and at a diameter of Ashley Davidoff MD TheCommonVein.net lungs-0744
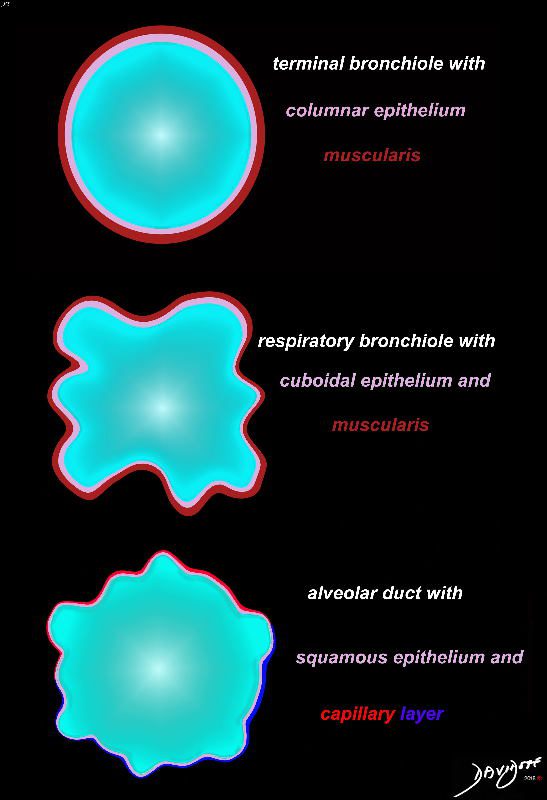
Cross section diagrams of the small airways. The top diagram shows a normal terminal bronchiole with columnar epithelium (pink), and muscularis (maroon). The respiratory bronchiole starts to have features of evolving respiratory airways, and he mucosa becomes cuboidal with persistence of the muscularis.
The alveolar duct has a squamous epithelium (pink), and is surrounded by a capillary network (blue – arteriolar component, and red venular component)
Ashley Davidoff MD thecommonvein.net lungs-0776b
Ashley Davidoff MD TheCommonVein.net lungs-0722

Ashley Davidoff MD TheCommonVein.net wall 56 001
Ashley Davidoff MD TheCommonVein.net wall 56 002
Ashley Davidoff MD TheCommonVein.net wall 56 003
Ashley Davidoff MD TheCommonVein.net lungs-0733
- Disease
- COPD 75-85% have small airway disease
- airway remodelling
- mucus plugging
- immune cell infiltration
- Inflammatory Disease
- Acute
- Hypersensitivity Pneumonitis
- Chronic
- RA
- Acute
- Infections
- Post Infectious
- Swyer james
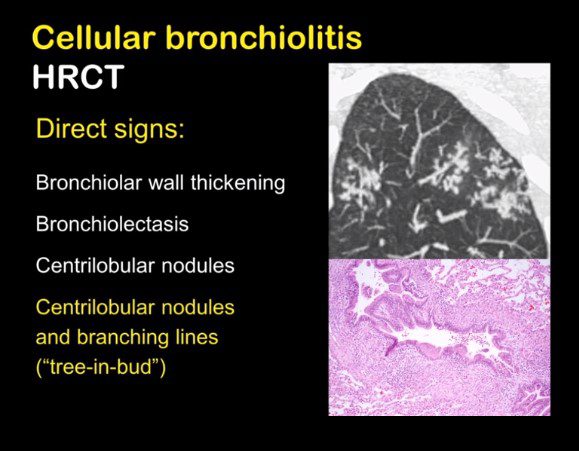
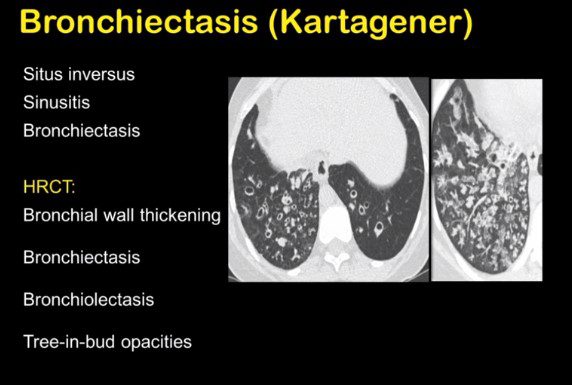
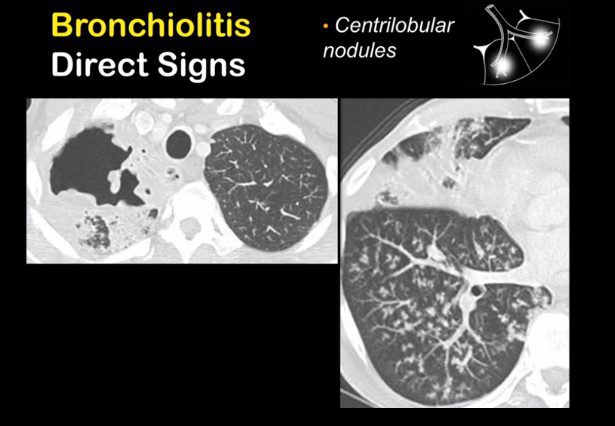
- Radiology
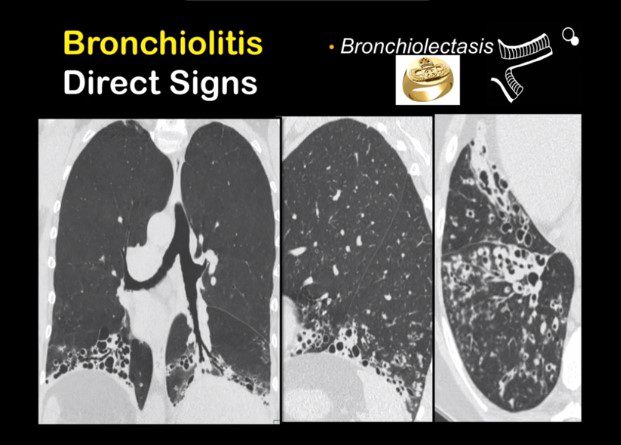
- Bronchiolar Wall Thickening
- Tree in Bud
- Centrilobular Nodules and Air Trapping
- Bronchiolectaisis
- bronchiectasis
- Low Caliber vessels
- Accentuation of Mosaic pattern on expiration
- Common Causes
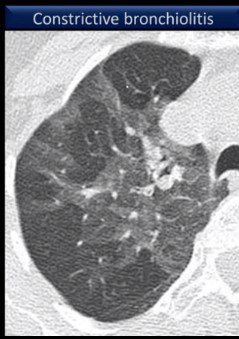
- Constrictive bronchiolitis
- post infectious
- patchy bilateral
- Swyer James/Macleod
- unilateral
- RA and other collagen vascular diseases
- Post lung transpalnt bronchiolitis obliterans syndromes
- Chronic Graft vs host
- post infectious
- Hypersensitivity Pneumonitis
- Poorly defined centrilobular Nodules
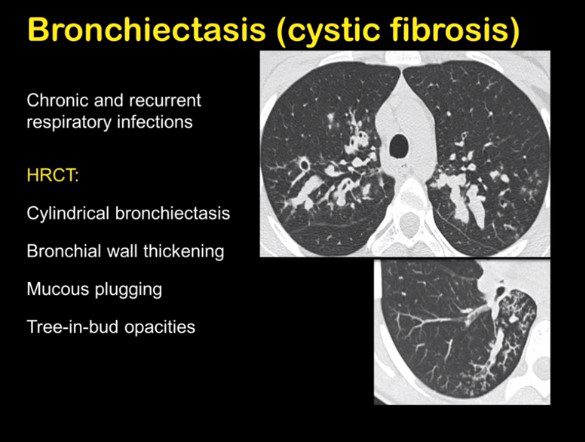
- Cystic Fibrosis
- Pulmonary Hypertension
- Constrictive bronchiolitis
- COPD 75-85% have small airway disease
Santiago Rossi ATS
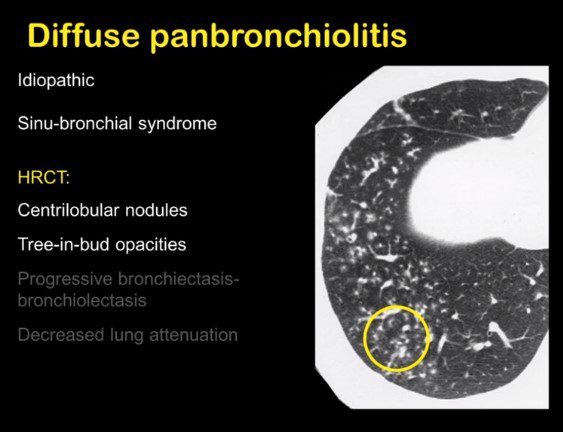
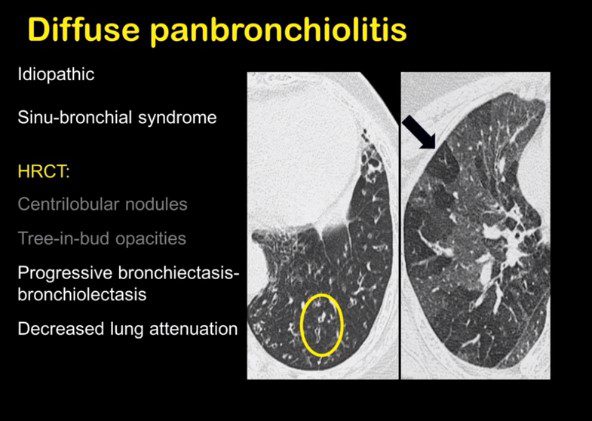
Society of Thoracic Radiology Santiago Rossi
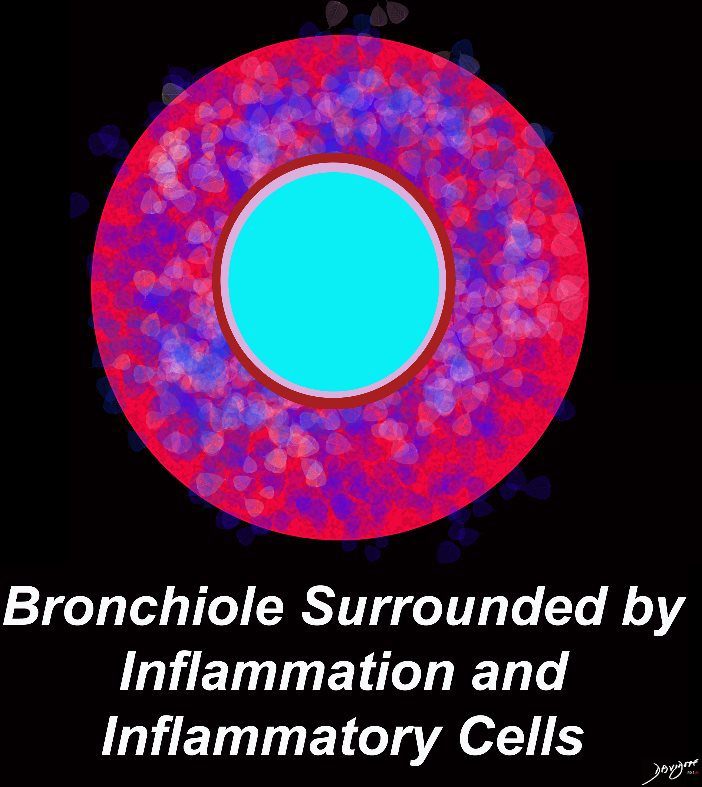
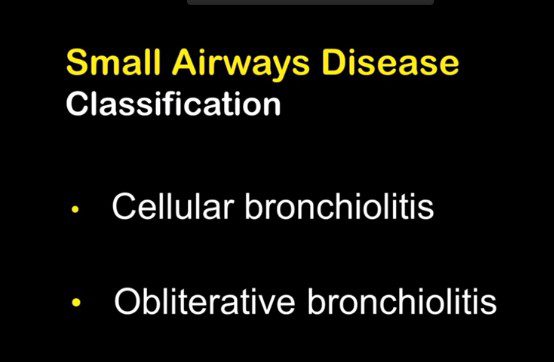
Bronchioles are rarely visible within 1cms of the pleural space
- When they become visible we have
- Inflammatory bronchiolitis
- Cellular Bronchiolitis

small airway disease ATS 003
Society of Thoracic Radiology Santiago Rossi
Mosaic Attenuation
Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi
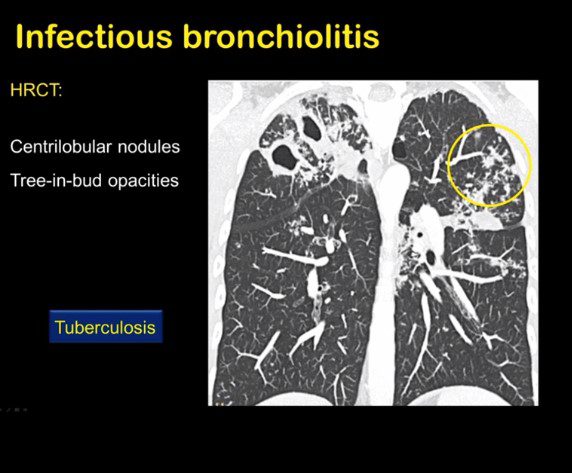
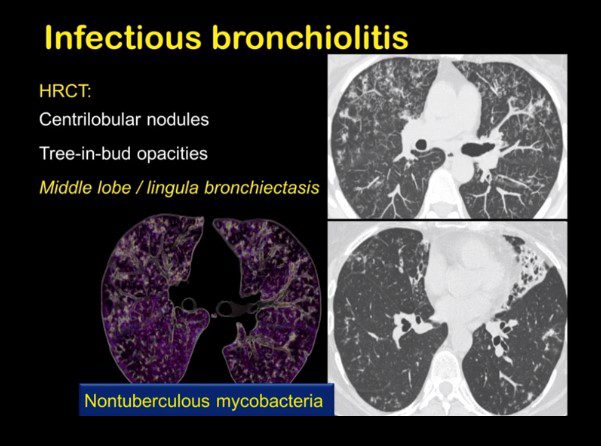
TB
Society of Thoracic Radiology Santiago Rossi

Society of Thoracic Radiology Santiago Rossi

Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi

Society of Thoracic Radiology Santiago Rossi
Society of Thoracic Radiology Santiago Rossi

Society of Thoracic Radiology Santiago Rossi
TB
Society of Thoracic Radiology Santiago Rossi
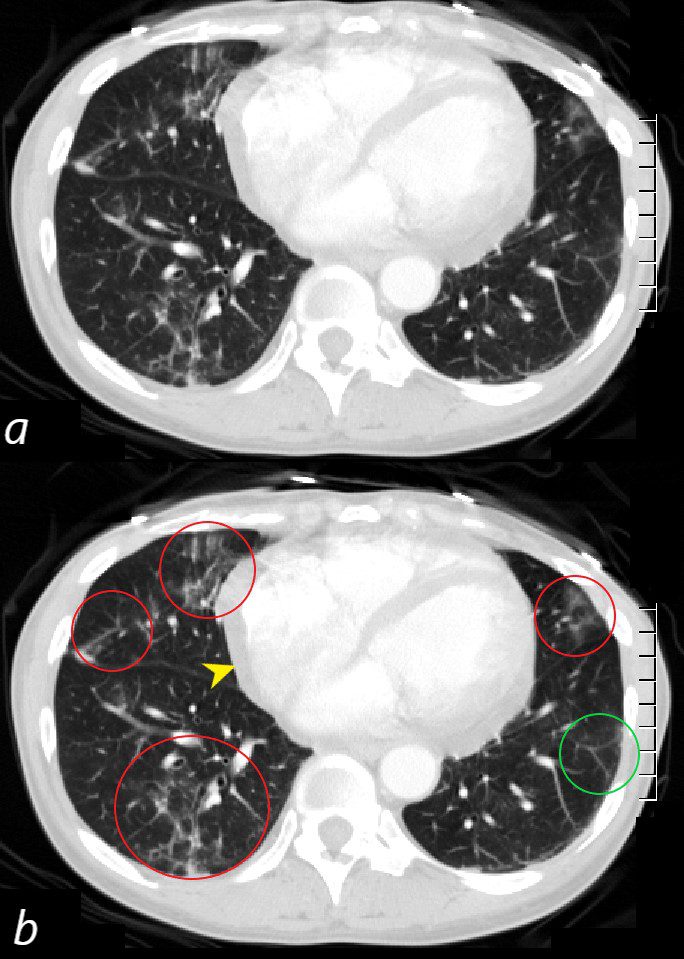
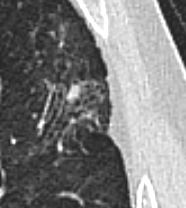
CT scan through the 4 chambers of the heart using lung windows is from a a 54 year old female with SLE. Recent CXR showed bibasilar ground glass infiltrates.
The scan shows basilar multicentric infiltrates with elements of ground glass change and small airway wall thickening (red circles in the right lower lobe middle lobe and lingula, as well as interlobular septal thickening (green circle) in the lateral basal segment of the left lower lobe. A small pericardial effusion is present (yellow arrowhead)
Ashley Davidoff MD
key words
SLE
acute pneumonitis
pericardial effusion
Burgel, P-R et al Small airways diseases, excluding asthma and COPD: an overview European Respiratory Review 2013 22: 131-147;
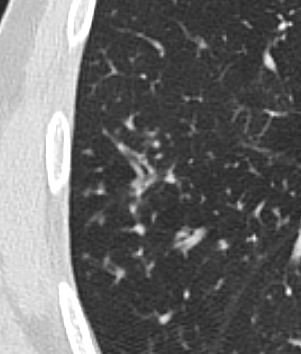
Mosaic Attenuation from Small Airways Disease

Small Airways are obstructed and air is trapped Sometimes small vessel disease, as in vasculltis, can lead to the air trapping
Ashley Davidoff MD TheCommonVein.net bronchioles 003

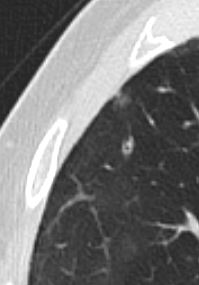
Small Airways and Smaller Airways are Filled with Mucus in a patient with COPD – Note Centrilobular Impaction of Mucus
Ashley Davidoff TheCommonVein.net bronchioles 004
Small Airways are obstructed and air is trapped Sometimes small vessel disease, as in vasculltis, can lead to the air trapping
Ashley Davidoff MD TheCommonVein.net bronchioles 002
Small Airways and Smaller Airways are Filled with Mucus in a patient with COPD – Note Centrilobular Impaction of Mucus
Ashley Davidoff TheCommonVein.net bronchioles 001
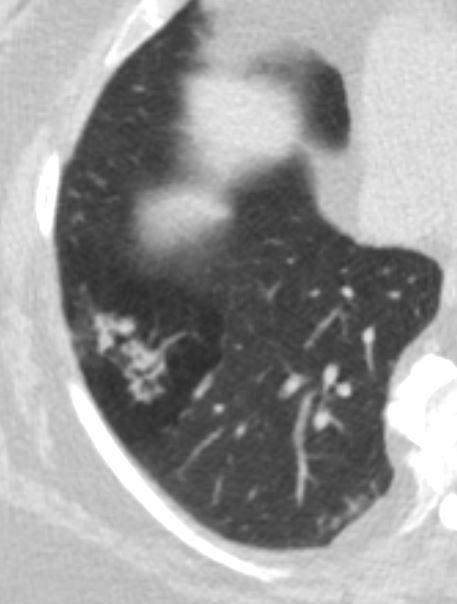
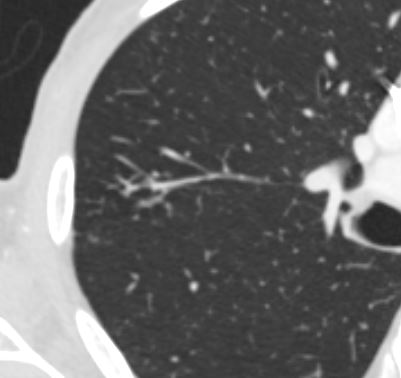
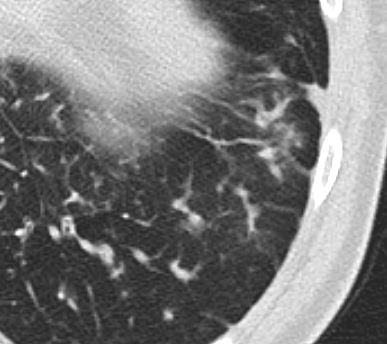
Representative images of computed tomography (CT) scans in patients with small airways disease. a) An inspiratory CT scan in a patient with hypersensitivity pneumonitis showing mosaic pattern of attenuation. b) Expiratory CT scan in the same patient showing air trapping that is characteristic of small airways disease. c) Ill-defined centrilobular nodules in a patient with farmer’s lung (personal communication; J.C. Dalphin). d) Localised micronodules branching with bronchovascular structures (tree-in-bud pattern) related to tuberculosis in a patient with rheumatoid arthritis receiving treatment with anti-tumour necrosis factor-α. Reproduced from [21] with permission from the publisher.
Burgel, P-R et al Small airways diseases, excluding asthma and COPD: an overview European Respiratory Review 2013 22: 131-147;
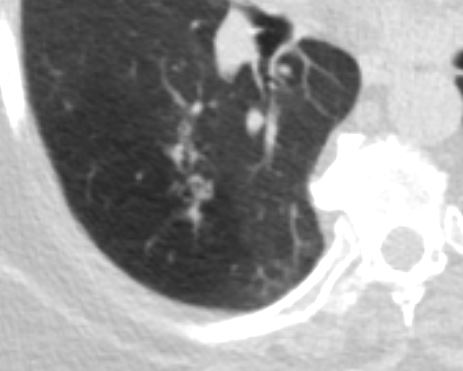
Broncholith

Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
ABPA
Ashley Davidoff MD TheCommonVein.net

Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
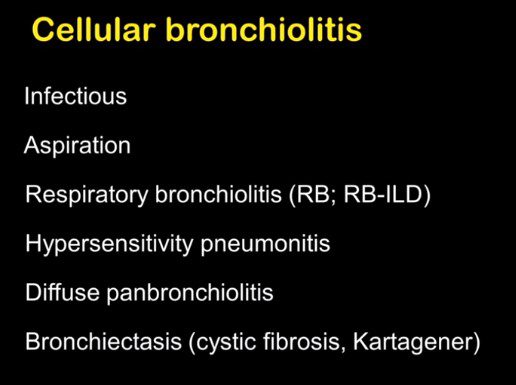
- Bronchiolar Inflammation
- AEIOU
- A
- Asthma ABPA Asbestosis
- E
- Eosinophilic Pneumonia
- Infections
- Endobronchial
- TB
- Mycobacterium
- Non TB Mycobacteria and
- Other Granulomatous Infections
- ABPA
- TB
- viruses such as
- adenovirus,
- influenza, and
- respiratory syncytial virus (RSV),
- Endobronchial
- Inflammatory
-
- Sarcoidosis
- Inhalational
- Cigarette Smoke
- smokers bronchiolitis
- Langerhans Cell
- chemicals,
- fumes, or toxic gases
- occupational exposures,
- industrial chemicals
- diacetyl in the popcorn industry
- industrial chemicals
- Cigarette Smoke
-
- Immune
-
-
- HP
- RA
- Follicular Bronchiolitis (MALT Lymphoid Hyperplasia in collagen vasc and immune deficiency)
- Graft vs Host
-
-
- Inherited
- Cystic Fibrosis
- Idiopathic Bronchiolitis Obliterans
- A
- AEIOU
Links and References
Burgel, P-R et al Small airways diseases, excluding asthma and COPD: an overview
Rossi Santiago Small Airway Disease
Rossi Santiago Case Based Hypersensitivity Pneumonitis You Tube
