-
Buzz
- Like sarcoid
- lymphatics and lymph nodes
- primary and secondary behave same way
- different
- age
- location
- Like sarcoid
Ashley Davidoff MD TheCommonVein.net lungs-0752
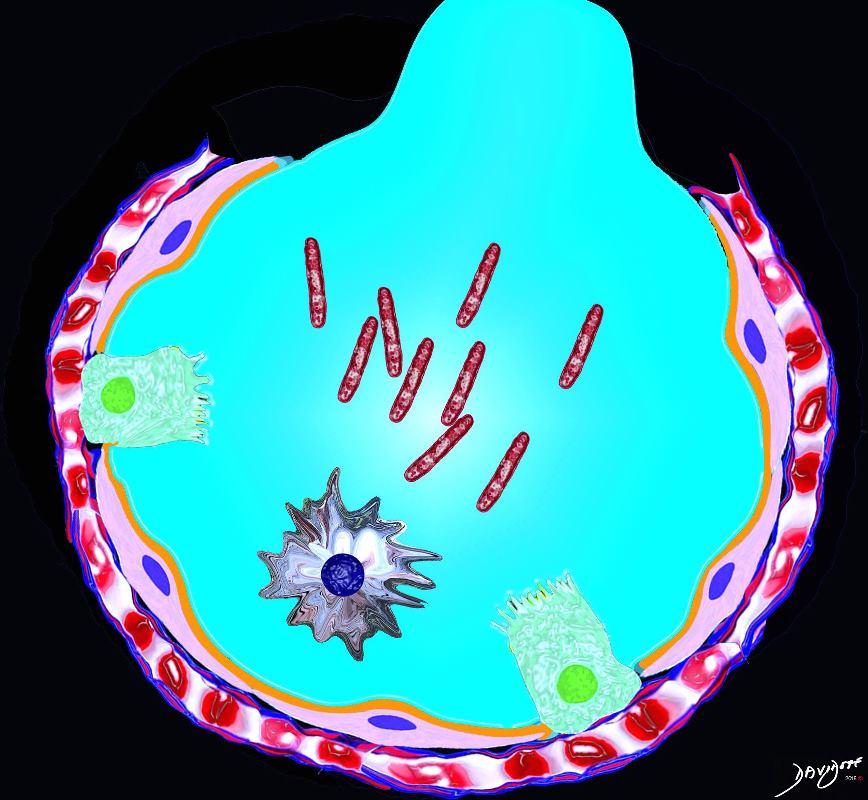
TB of the lung is an infection caused by mycobacterium TB with two phases – an activation phase and a reactivation phase adenopathy a
Inhaled droplets of Mycobacterium
Mycobacterium Tuberculosis (MTB)
- Etymology:
- The term “tuberculosis” derives from the Latin word “tuberculum,” referring to the nodular lesions (tubercles) seen in the disease.
- AKA:
- Tuberculosis
- TB
- MTB
- Koch’s Disease
- What is it?
- Mycobacterium tuberculosis (MTB) is a pathogenic bacterial species belonging to the Mycobacterium genus, primarily causing tuberculosis.
- It is an obligate aerobe and a slow-growing, acid-fast bacillus.
- Types of Mycobacteria:
- Mycobacterium tuberculosis
- Mycobacterium bovis (bovine tuberculosis)
- Mycobacterium leprae (leprosy)
- Mycobacterium africanum
- Mycobacterium microti
- Nontuberculous Mycobacteria (NTM) such as Mycobacterium avium complex (MAC)
- Caused by:
- Infection with Mycobacterium tuberculosis, transmitted via airborne droplets.
- Distinction between Latent TB (LTBI) and Active Disease:
- LTBI:
- Asymptomatic
- Positive TST or IGRA
- No radiographic evidence of active disease
- Not infectious
- Active TB:
- Symptomatic with cough, fever, night sweats, and weight loss
- Radiographic findings such as cavitation, miliary nodules
- Infectious
- LTBI:
- Forms of Active TB Disease:
- Pulmonary TB:
- Most common form
- Cavitation, consolidation, tree-in-bud nodules
- Miliary TB:
- Hematogenous spread leading to widespread tiny nodules
- Severe form with systemic involvement
- Endobronchial TB:
- Spread within the airways
- Bronchial wall thickening and narrowing
- Disseminated TB:
- Involvement of multiple organs
- Often seen in immunocompromised patients
- Pulmonary TB:
- Structural Changes:
- Formation of granulomas
- Caseating necrosis
- Cavitary lesions
- Pathophysiology:
- MTB infects alveolar macrophages.
- The bacteria can evade immune destruction and form granulomas.
- Latent TB can persist for years without symptoms but may reactivate.
- Pathology:
- Granulomas with central caseation
- Acid-fast bacilli (AFB) on staining
- Diagnosis:
- Tuberculin skin test (TST)
- Interferon-gamma release assays (IGRAs)
- Chest X-ray
- Sputum AFB smear and culture
- NAAT and PCR tests
- Clinical:
- Chronic cough
- Hemoptysis
- Night sweats
- Fever
- Weight loss
- Radiology:
- Latent TB:
- CXR:
- Parts: Typically normal or may show calcified granulomas
- Size: Small calcified nodules
- Shape: Round or oval, with possible retraction of hila and linear nodular changes
- Position: Upper lobes or apices
- Character: Non-progressive, with calcified granulomas
- Associated Findings: Fibrosis, pleural thickening, volume loss, and lymphadenopathy (LAD)
- CT:
- Parts: Lungs, often upper lobe involvement with parenchyma and airway involvement
- Size: Small nodules, <5mm
- Shape: Nodular with linear and nodular changes, architectural distortion, and hilar retraction
- Position: Apical and upper lobes, but diffuse in miliary disease
- Character: Calcification, fibrosis, cicatricial atelectasis, bronchiectasis,
- Associated Findings: Fibrosis, pleural thickening, volume loss, and lymphadenopathy (LAD)
- CXR:
- Latent TB:
- Distinction from NTM:
- MTB is primarily a human pathogen, while NTM species are environmental.
- MTB often presents with caseating granulomas, while NTM typically involves non-caseating granulomas.
- MTB is transmissible person-to-person; NTM is generally not transmissible.
- Labs:
- Latent TB:
- Tuberculin Skin Test (TST)
- Interferon-Gamma Release Assays (IGRAs)
- Active TB:
- Positive sputum AFB smear and culture
- Positive NAAT for MTB
- Elevated ESR and CRP
- Chest X-ray
- CT Scan
- Latent TB:
- Management:
-
- Management:
- Latent TB:
-
-
The criteria for diagnosing LTBI include:1. Positive Tuberculin Skin Test (TST):2. Positive Interferon-Gamma Release Assay (IGRA):
- Isoniazid (INH) monotherapy for 6-9 months
- Rifampin (RIF) for 4 months (alternative regimen)
- Isoniazid and Rifapentine weekly for 3 months (3HP regimen)
-
The American Thoracic Society (ATS), Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) recommend treating latent TB infection to prevent the progression to active TB disease. This is particularly important in individuals with a positive tuberculin skin test (TST) or interferon-γ release assay (IGRA) who are at increased risk for developing active TB, such as those with HIV infection or other immunocompromising conditions.For HIV-infected individuals, the U.S. Public Health Service and IDSA guidelines recommend treatment for latent TB infection if they have a positive TST result (≥5 mm of induration) and no evidence of active TB. Treatment options include isoniazid daily or twice weekly for 9 months, or 4 months of daily rifampin.[2]The rationale for treating latent TB is to reduce the risk of reactivation and subsequent transmission of TB. This approach is supported by evidence showing that untreated latent TB can lead to active TB, which has significant public health implications.
-
- Active TB:
- First-line anti-TB therapy:
- Isoniazid (INH)
- Rifampin (RIF)
- Pyrazinamide (PZA)
- Ethambutol (EMB)
- Directly observed therapy (DOT) recommended
- Prolonged treatment for multidrug-resistant TB (MDR-TB)
- First-line anti-TB therapy:
- Management:
-
- Pulmonary Function Tests (PFTs):
- Not commonly performed but can show restrictive patterns in advanced disease
- Recommendations:
- Confirm diagnosis with microbiological testing
- Use standard four-drug therapy for active TB
- Latent TB infection should be treated with isoniazid or rifampin
- Key Points and Pearls:
- MTB is primarily an airborne pathogen
- Cavitary lesions are more typical of post-primary TB
- Miliary TB presents as diffuse tiny nodules
- Citations:
- WHO. Global Tuberculosis Report 2021.
- Centers for Disease Control and Prevention (CDC). Tuberculosis.
- Sharma SK, Mohan A. Tuberculosis. Indian J Med Res. 2004;120(4):248-276.
- Immediate clearance of the organism
- Primary disease: immediate onset of active disease
- Latent infection
-

Position of Disease
Upper and mid lung field distribution
Ashley Davidoff MD TheCommonvein.net lungs-0772 - Reactivation disease: onset of active disease many years following a period of latent infection
- Consolidation
- Cavitation
- Miliary
key Dx feature upper or Rt middle lobe involvement initial exudative phase, vol loss instead of exp hypersensitivity rxn causes chronic inflam phase caseation necrosis after 6 wks
Radiology
Primary tuberculosis demonstrates
lymphadenopathy,
consolidation, (CAVITATION UNCOMMON)
pleural effusion, and
miliary nodules
middle lobes
upper portion of lower lobes or lower portion of upper lobes
Ghon lesion, sometimes called Ghon focus,
initial tuberculous granuloma formed during primary infection and is not radiologically visible unless it calcifies – this occurs
represents a tuberculous caseating granuloma (tuberculoma) and represents the sequelae of primary pulmonary tuberculosis infection.
Ghon complex.
is a Ghon focus alongside ipsilateral mediastinal lymphadenopathy
Ranke complex
is calcified Ghon complex (Ghon lesion and ipsilateral lymph node) representing a progression of the Ghon complex
radiologically detectable
-
Feature Mycobacterium tuberculosis (MTB) Atypical Mycobacterium (NTM- Non Tuberculous Mycobacteria) eg avium-intracellulare (MAC)
Pathogen Type Mycobacterium tuberculosis complex (MTB) Mycobacterium avium and Mycobacterium intracellulare Transmission Human-to-human via airborne droplets Environmental exposure (soil, water, aerosols) Primary Reservoir Humans Environment (soil, water, birds, animals) Virulence and Pathogenicity Highly virulent, infects healthy individuals Opportunistic, primarily affects immunocompromised patients (HIV/AIDS) Primary Affected Population General population, especially in endemic areas Immunocompromised patients (e.g., HIV/AIDS, elderly with structural lung disease) Clinical Presentation Fever, night sweats, cough, hemoptysis, weight loss Chronic cough, fatigue, weight loss, occasional hemoptysis Pulmonary Involvement Cavitary lesions, consolidation, apical nodules Bronchiectasis, nodular opacities, tree-in-bud pattern CXR Features Upper lobe cavitation, consolidation, nodules, apical fibrosis Middle lobe and lingula involvement, nodular opacities, tree-in-bud pattern CT Features – Upper lobe predominant cavitation, apical scarring, tree-in-bud opacities
– Patchy consolidation, centrilobular nodules– Middle lobe and lingula nodular opacities
– Bronchiectasis with mucus plugging
– Tree-in-bud nodularityExtrapulmonary Involvement Common (e.g., lymph nodes, CNS, bones, GI tract) Rare, mainly disseminated in immunocompromised hosts Histopathology Caseating granulomas, Langhans giant cells Non-caseating granulomas or granuloma absence Diagnosis Sputum AFB smear, culture, PCR (GeneXpert) Sputum culture, PCR, MAC-specific NAAT Infectiousness Highly contagious Not contagious between humans Drug Susceptibility Requires prolonged treatment, MDR strains exist Less drug resistance compared to MTB First-line Treatment Isoniazid (INH), Rifampin (RIF), Pyrazinamide (PZA), Ethambutol (EMB) Clarithromycin or Azithromycin + Ethambutol, Rifabutin Treatment Duration 6-9 months (18 months for MDR-TB) 12-18 months or until culture negative for 12 months Prevention BCG vaccination, infection control measures Avoidance of environmental exposure (e.g., contaminated water) Geographical Distribution Endemic in developing countries Worldwide, especially in immunocompromised patients Complications Miliary TB, tuberculomas, Pott’s disease Disseminated disease in AIDS, MAC lung disease Immune Response Delayed-type hypersensitivity (DTH), granuloma formation Weak immune response, especially in immunocompromised
- 30 year old Female with Positive Sputum
- multiple tree-in-bud opacities and nodules
- measuring up to 8 mm in
- peribronchial vascular distribution in the
- left upper lobe the,
- lingula,
- left lower lobe,
- withslight surrounding groundglass.
- several bilateral calcified granulomas.
- CXR showed
-

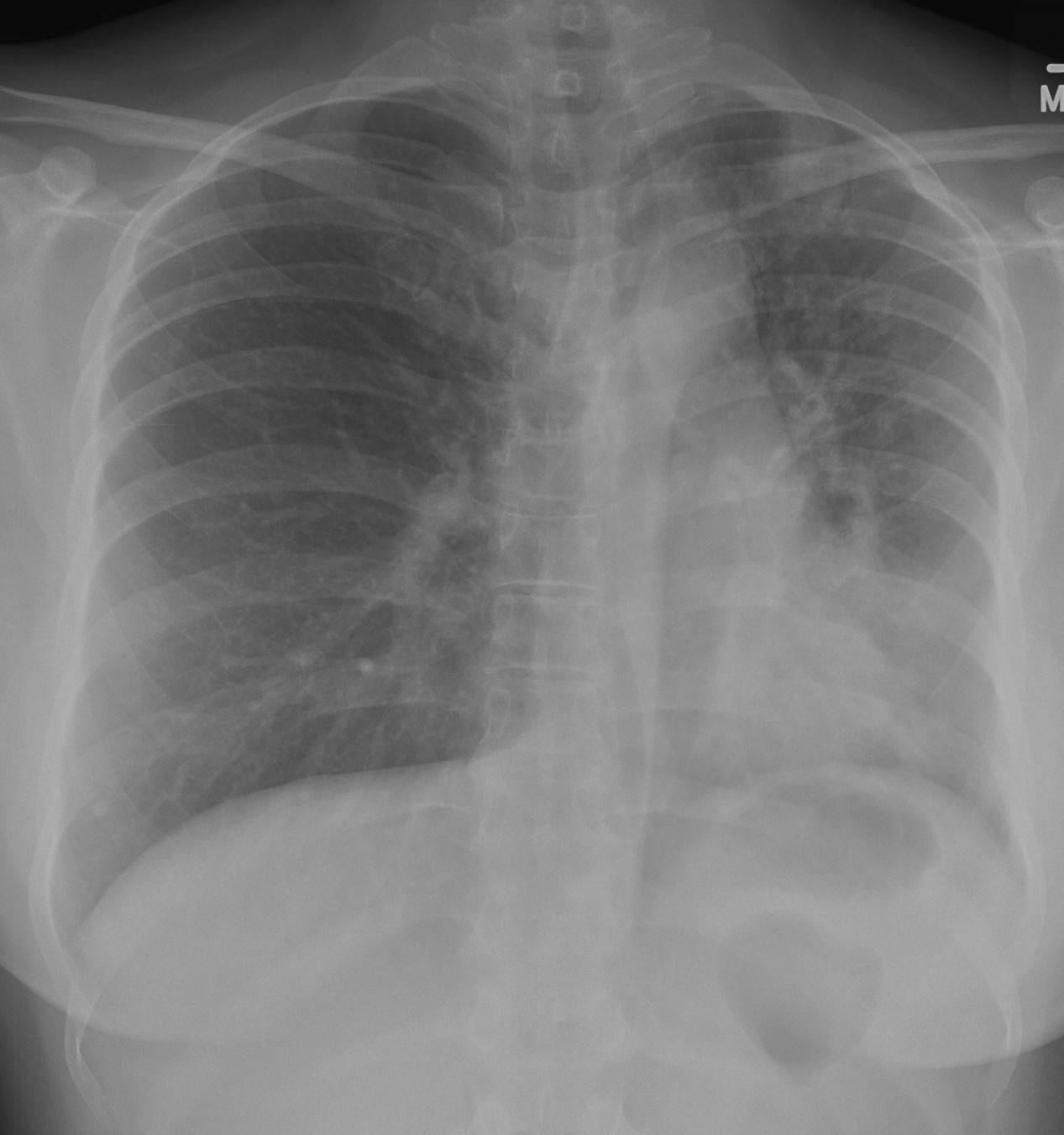
Acute on Latent TB 46 f with positive sputum LUL nodules tree in bud and GGO on CT
CXR shows volume loss with tracheal shift mild elevation of the left hemidiapgragm left lower lobe, lingular and less obvious left upper lobe infiltrate and granulomas right base
Ashley Davidoff MD TheCommonVein.net
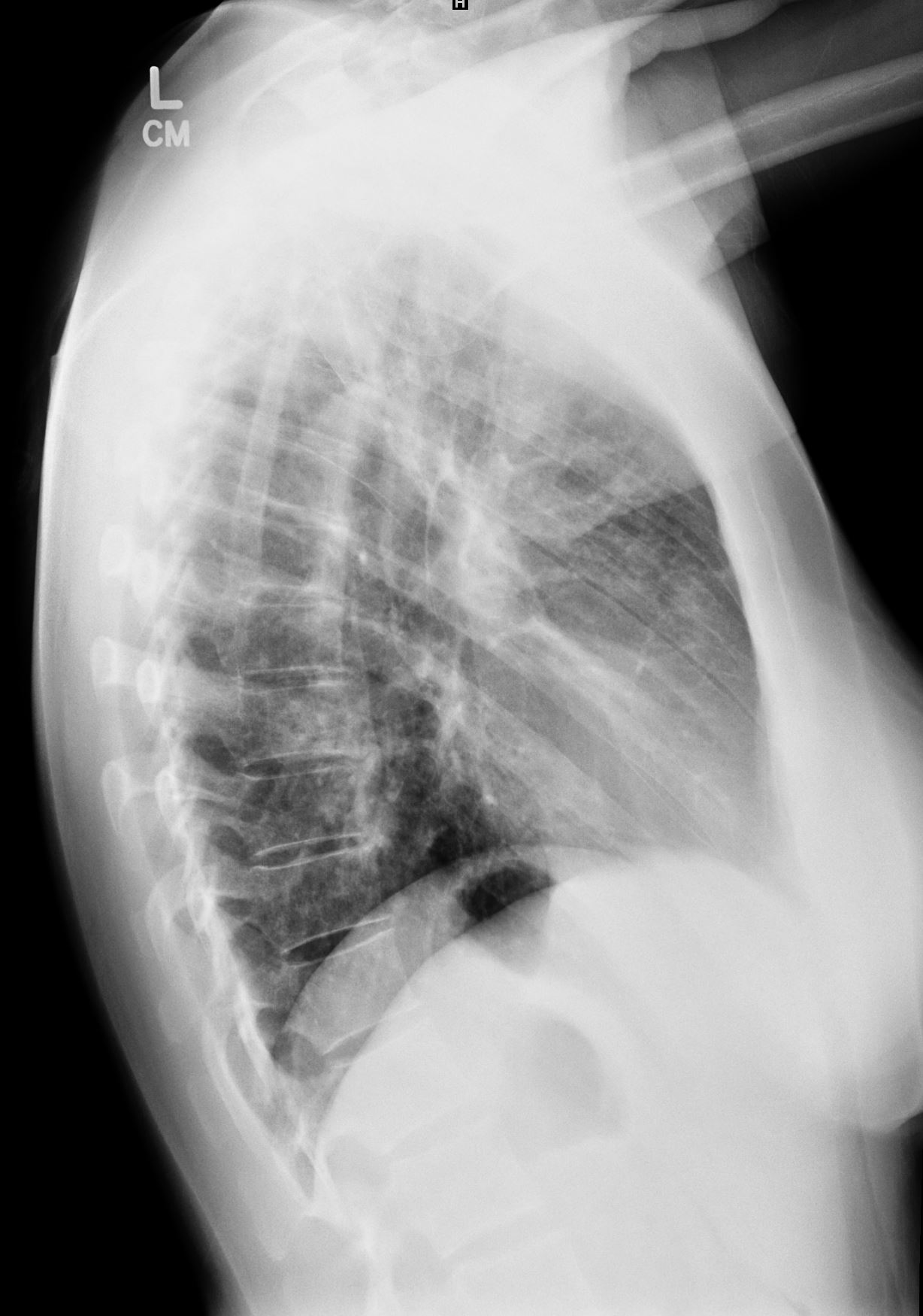
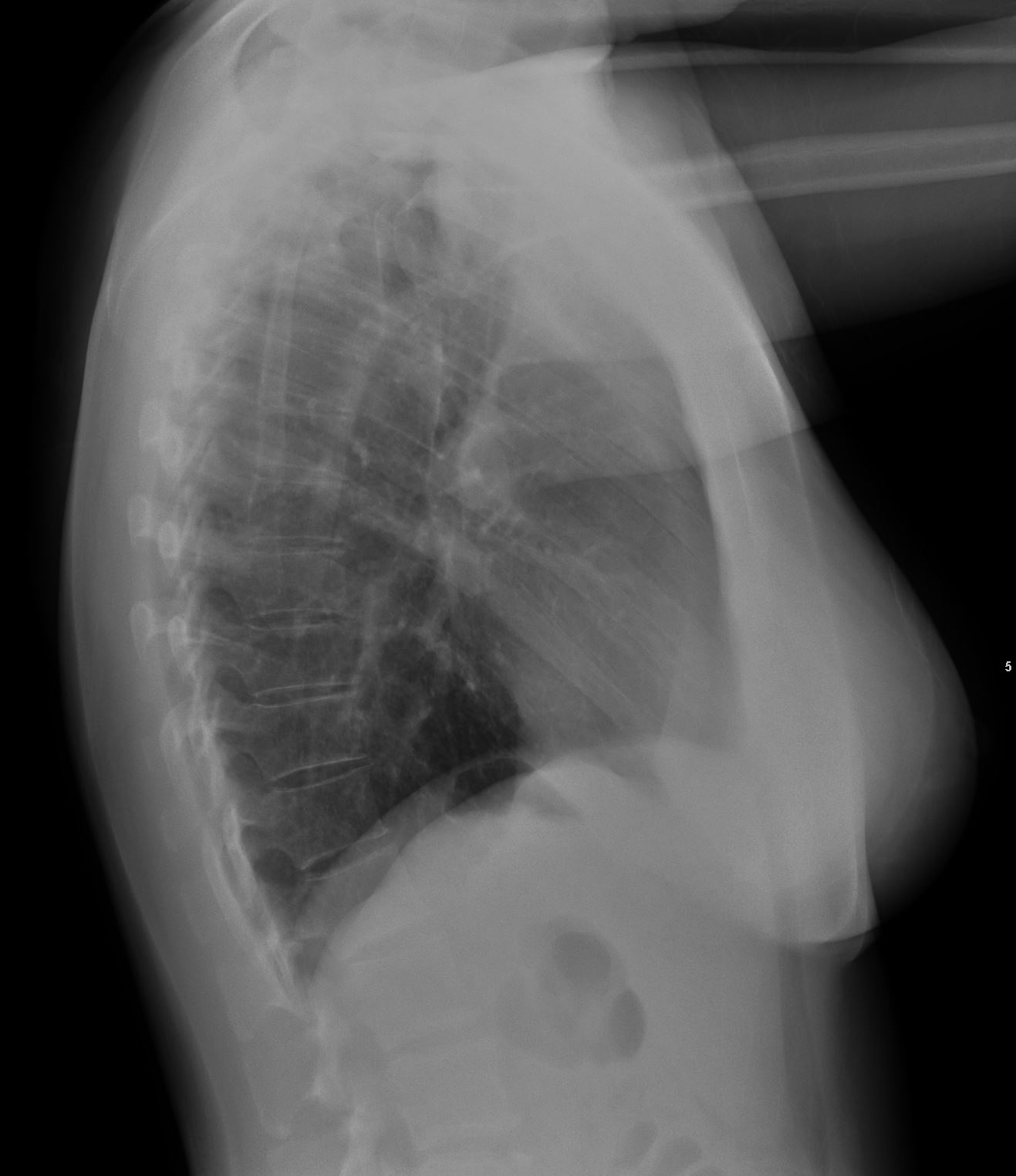
Acute on Latent TB 46f with positive sputum LUL nodules tree in bud and GGO on CT Lateral CXR shows mild elevation of the left hemidiapgragm subsegmental left lower lobe, lingular and lreticulonodular changes in the anterior segment of the LUL and lingula
Ashley Davidoff MD TheCommonVein.net3 Months Later on Treatment
-

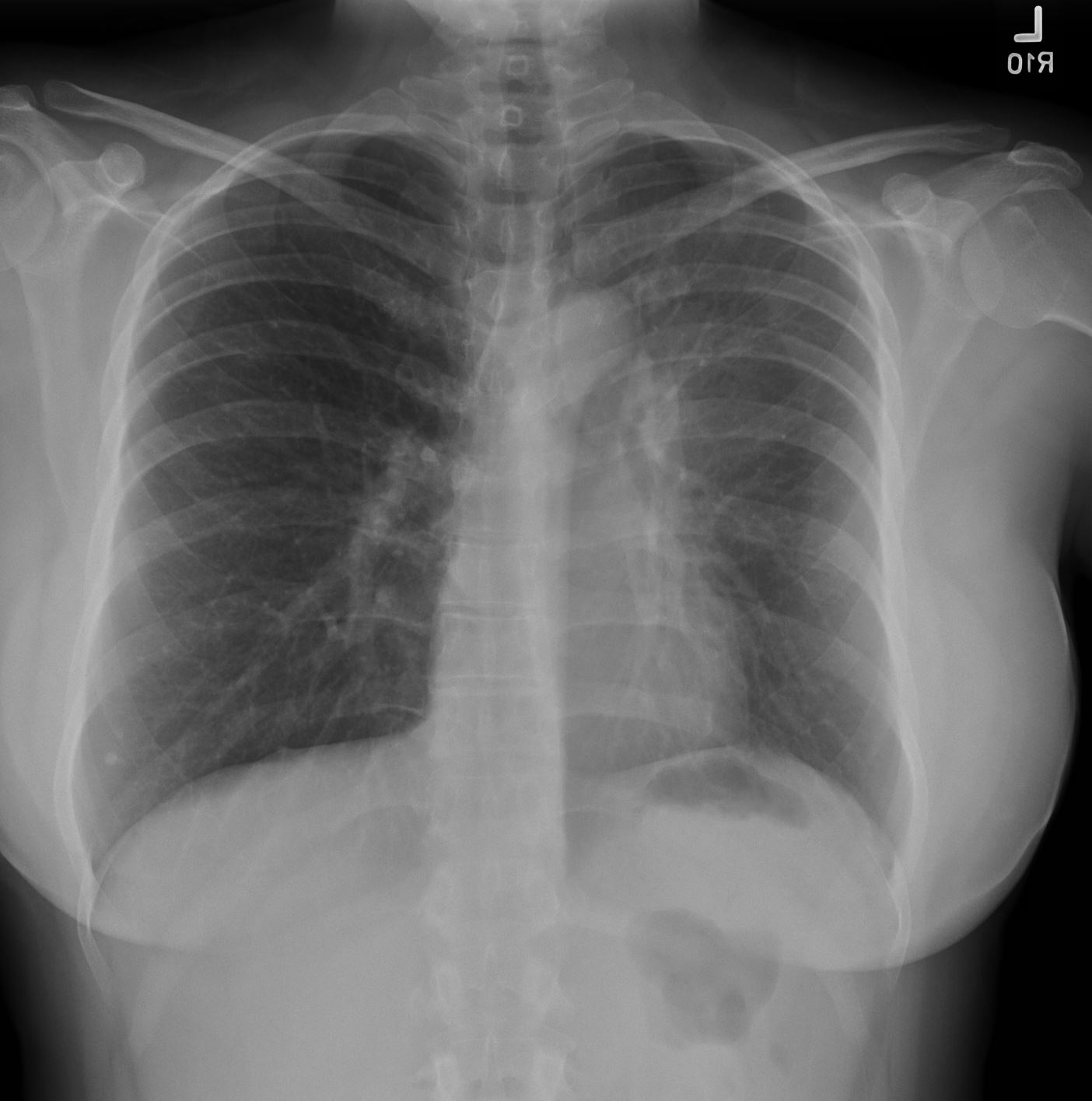
Acute on Latent TB following 3 months treatment
CXR is significantly improved with resolution of infiltrates in the left lower lobe and lingula and with retraction of the left hilum and crowding of the markings in the LUL . There is persistent volume loss with elevation of the left hemidiaphragm and rightward deviation of the trachea . Granulomas noted atthe right base Ashley Davidoff MD TheCommonVein.net
Acute on Latent TB following 3 months treatment
CXR significantly improved with resolution of infiltrates in the left lower lobe and lingula
Ashley Davidoff MD TheCommonVein.net
-
- multiple tree-in-bud opacities and nodules
CT showed
Postprimary tuberculosis
(aka – reactivation TB and secondary TB)
consolidations that are predominant in the apical and upper lung zones,
nodules, and
cavitation
-

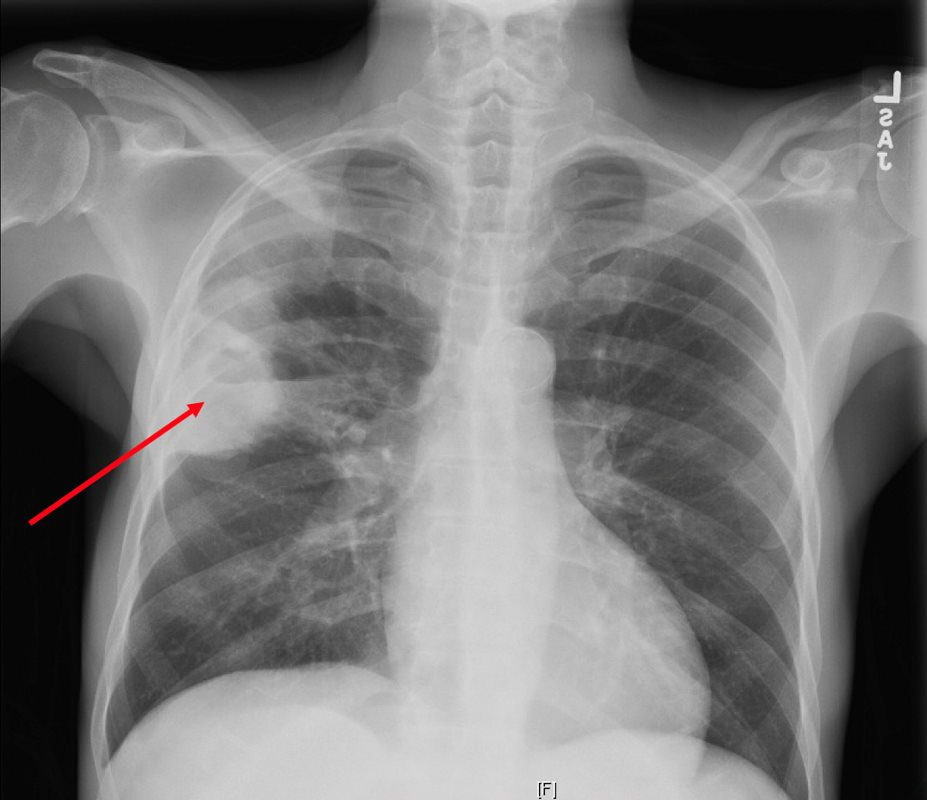
Reactivation TB
CXR reveals a dense consolidation in the right upper lobe (red arrow) with questionable air-fluid level. No pneumothorax. No pleural effusions. Differential includes right upper lobe pneumonia or tuberculosis. CT is recommended for further evaluation if there is concern for a cavity.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
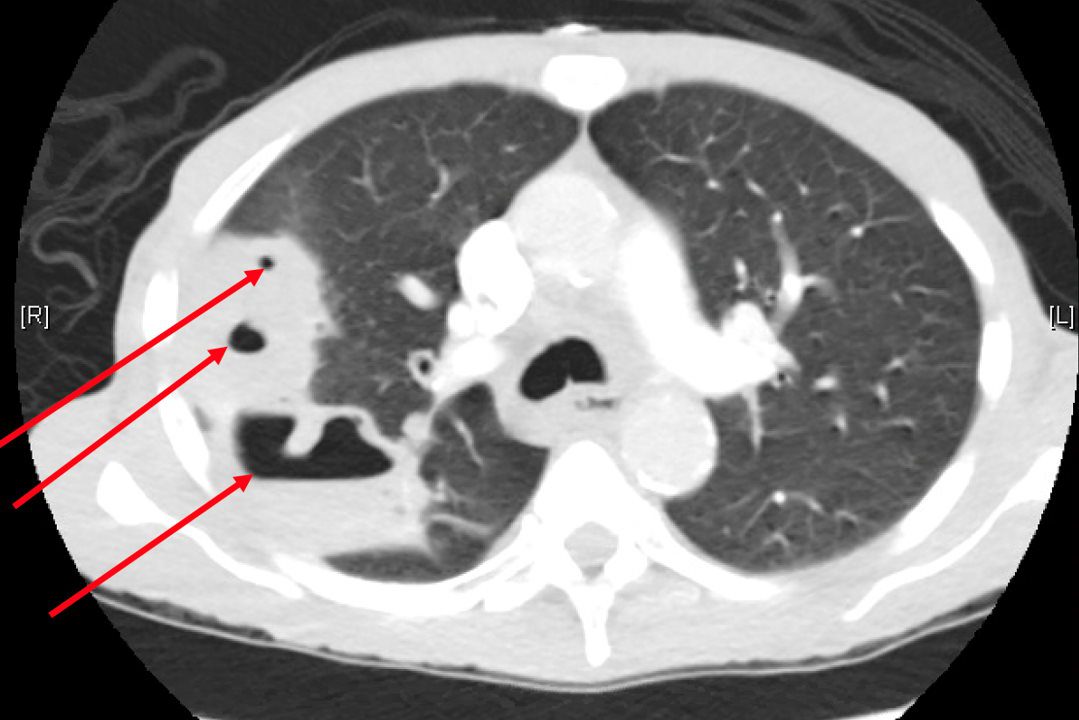
CTPA reveals a large consolidation in the right upper lobe and superior segment of the right lower lobe spans approximately 8.8 x 5.6 x 9.4 cm and extends to the pleura. There are multiple internal cavitations (red arrows) with air-fluid levels. These large predominately right upper lobe cavitary lesions are consistent with clinical concern for tuberculosis pneumonia, however follow-up with chest CT in 3 months post-treatment is recommended to exclude other less likely causes of cavitary lesions, such as malignancy.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
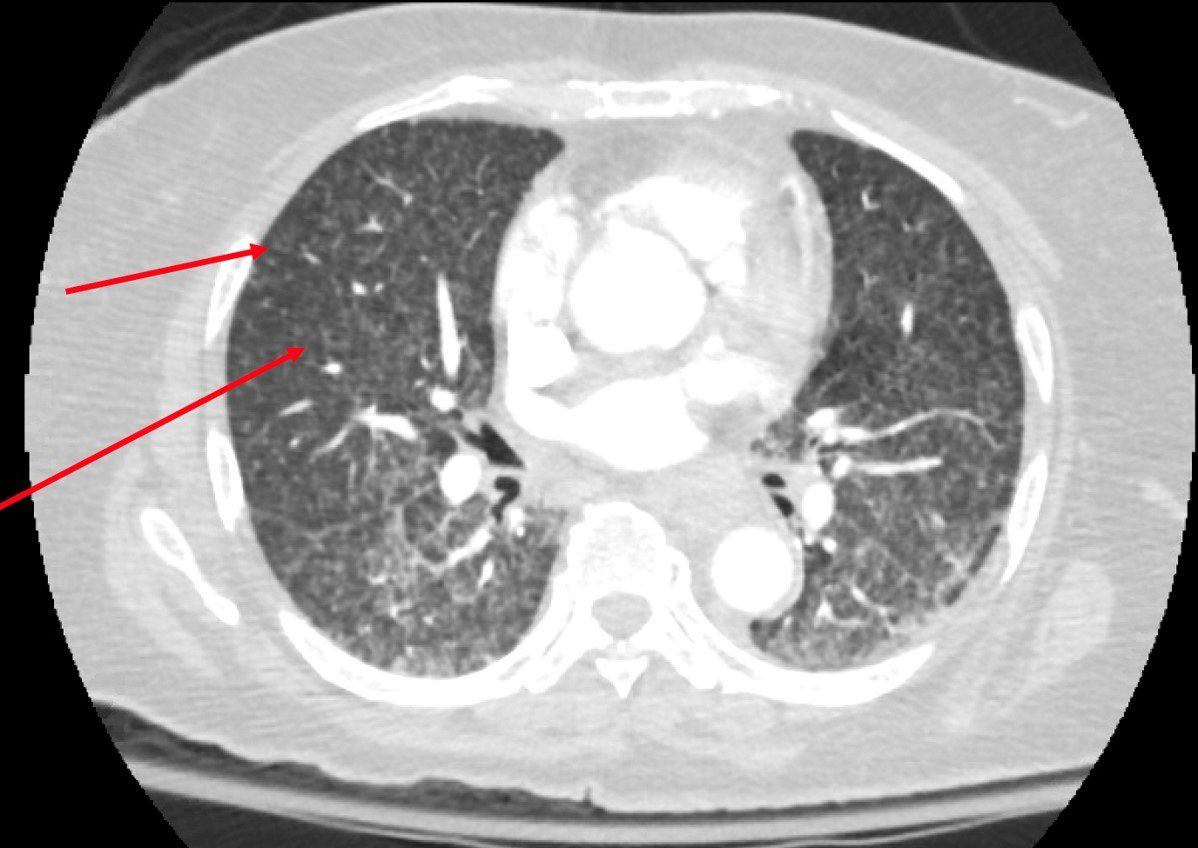
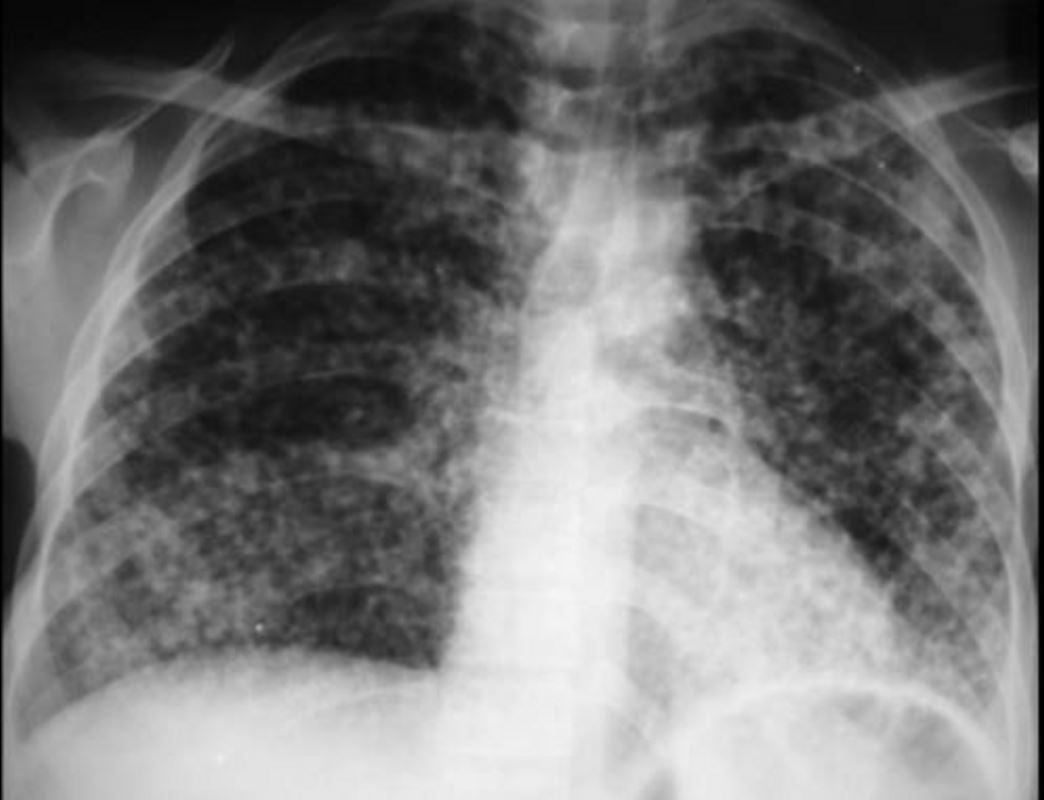
Miliary TB
CTPA reveals innumerable punctate nodules in a randomly distribution (red arrows). There are areas of groundglass opacity predominantly in a central peribronchial vascular distribution in both lungs. No pneumothorax. Differential of innumerable punctate nodules is consistent with miliary TB.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
CT reveals bulky conglomerate lymphadenopathy with central hypodensity (red arrow) in right levels IV, VI, supraclavicular region and partially visualized within the upper mediastinum. Differential includes infection, such as mycobacterial, or malignancy.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
CT –CAP in the sagittal projection shows extensive lytic lesions of the T11 (red arrow) and L2 (green arrow) vertebral bodies. In addition, there is an extensive lytic lesion from S2 inferiorly (blue arrow) with an associated soft tissue mass. There are no additional lesions in the thoracic or lumbar spine. These findings may represent metastatic disease, or possibly an infectious etiology such as tuberculosis.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MSActive TB
-
- as primary tuberculosis, developing shortly after infection,
- or postprimary tuberculosis
- Stability of radiographic findings for 6 months distinguishes inactive from active disease
- Primary Active
-
-
- lymphadenopathy,
- consolidation,
- pleural effusion, and
- miliary nodules
-
-
- Reactivation
- consolidations that are predominant in the apical and upper lung zones,
- nodules
- tree in bud
- cavitation
-
Primary Active and Reactivation
miliary tuberculosis is evenly distributed throughout both lungs
Courtesy https://www.slideshare.net/

82 year old man s/pthoracoplasty for treatment of right upper lobe TB. Associated finding is left ventricular enlargement
Ashley Davidoff MD
References and Links
- Radiographics
- Nachiappan, A.C et al Pulmonary Tuberculosis: Role of Radiology in Diagnosis and Management RadioGraphicsVol. 37, No. 1 2017
- Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphicsVol. 25, No. 3 2005
-
Bhalla, A S et al Chest tuberculosis: Radiological review and imaging recommendation Indian J Radiol Imaging. 2015 Jul-Sep; 25(3): 213–225.
- Radiopaedia
-
TCV