-
- Etymology
- Derived from the Greek words “trachea,” meaning rough artery or windpipe, and “malakia,” meaning softness.
- AKA
- None commonly used.
- What is it?
- Tracheomalacia refers to the abnormal softening of the tracheal cartilage.
- It results in increased tracheal wall compliance, leading to dynamic collapse of the trachea during the respiratory cycle.
- Characterized by
- Collapse of the tracheal lumen by more than 50% during exhalation.
- Symptoms such as cough, wheezing, dyspnea, and stridor.
- Can be congenital or acquired.
- Anatomically affecting
- The trachea, particularly the intrathoracic segment.
- Causes include
- Most Common Causes
- Congenital cartilage defects.
- Prolonged mechanical ventilation or tracheostomy.
- Other Causes include:
- Infection: Recurrent respiratory infections.
- Inflammation: Chronic obstructive pulmonary disease (COPD), relapsing polychondritis.
- Trauma: Blunt trauma, surgery.
- Mechanical: Compression by tumors or vascular anomalies.
- Idiopathic: Unknown etiology.
- Iatrogenic: Complications of prolonged intubation.
- Most Common Causes
- Pathophysiology
- Weakening of the tracheal cartilage leads to dynamic narrowing of the airway.
- Exacerbated during exhalation when intrathoracic pressure increases.
- Histopathology
- Loss of cartilage integrity with thinning or degeneration.
- Hyaline cartilage replacement with fibrous tissue in some cases.
- Imaging Radiology
- Applied Anatomy to CT
- Parts: Visible as the tracheal lumen and surrounding cartilage.
- Size: Reduced cross-sectional area of the trachea during exhalation.
- Shape: Crescentic or elliptical lumen collapse.
- Position: Most commonly involves the intrathoracic trachea.
- Character: Dynamic collapse of the tracheal walls seen on inspiratory and expiratory CT.
- Time: Exacerbation during forced expiration or coughing.
- CXR
- Typically not diagnostic but may show associated conditions like air trapping or hyperinflation in severe cases.
- CT
- Inspiratory and expiratory high-resolution CT is the gold standard for evaluation.
- Demonstrates excessive narrowing of the tracheal lumen (>50%) during exhalation.
- May show associated airway abnormalities like bronchiectasis or mucus plugging.
- MRI
- Rarely used but may provide information on adjacent soft tissue structures.
- Dynamic Bronchoscopy
- The definitive diagnostic test, directly visualizing tracheal collapse during respiration.
- Nuclear Medicine
- Not typically utilized but can show secondary ventilation-perfusion mismatch in severe cases.
- Applied Anatomy to CT
- Differential Diagnosis
- Bronchomalacia.
- Fixed tracheal stenosis.
- Tracheobronchopathia osteochondroplastica.
- Relapsing polychondritis.
- Recommendations
- Dynamic inspiratory and expiratory CT to confirm the diagnosis.
- Bronchoscopy for direct visualization and possible therapeutic interventions.
- Key Points and Pearls
- Tracheomalacia is best evaluated with dynamic imaging techniques.
- Symptomatic cases may require stenting or surgical correction.
- Parallels with Human Endeavors
- Represents structural failure, akin to a bridge with weakened supports collapsing under weight.
- Etymology
Tracheomalacia is a condition characterized by weakness and
excessive flexibility of the tracheal cartilage, leading to the collapse
of the trachea during breathing, especially on exhalation. This
results in airway obstruction and symptoms such as chronic cough,
wheezing, stridor, and difficulty breathing. Tracheomalacia can be
congenital, where it is present at birth due to underdeveloped
tracheal cartilage, or acquired, often resulting from prolonged
intubation, tracheal injury, or chronic inflammation from conditions
like chronic obstructive pulmonary disease (COPD) or
tracheobronchitis. Diagnosis is typically made using bronchoscopy,
which allows direct visualization of tracheal collapse, or through
dynamic CT scans that show airway narrowing during breathing.
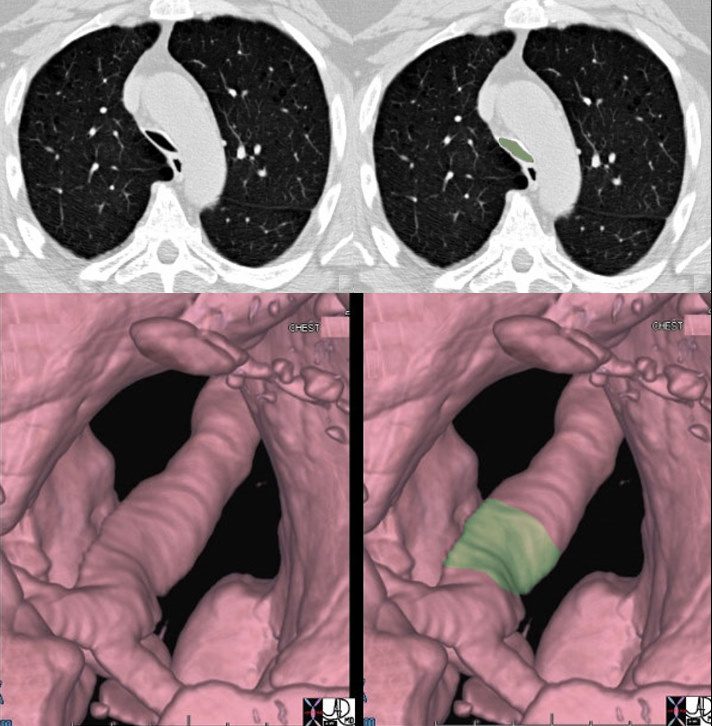
The trachea narrows significantly in its A-P dimension above the carina as seen in the cross sectional CT (a,b) with th narrowing noted in green overlay, and the change in diameter is better appreciated in the surface rendering of the trachea in c and d.
46114c04 Ashley Davidoff TheCommonVein.net
68 year female with tracheomalacia
On inspiration the trachea is normal and widely patent and on expiratation the trachea collapses to greater than 50% of its original diameter
Ashley DAvidoff MD
TheCommonVein.net
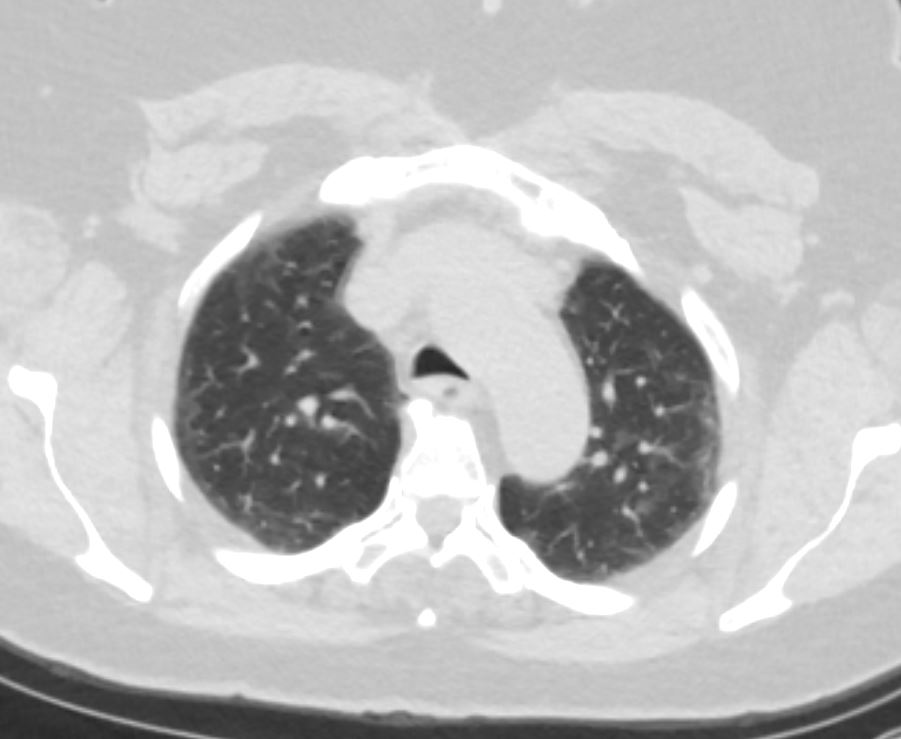
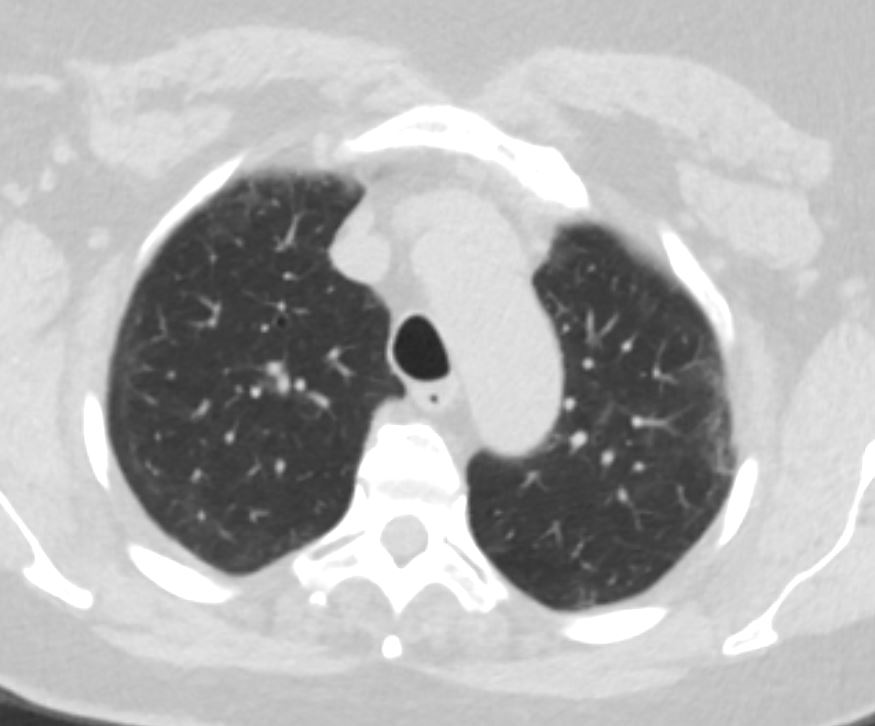
68 year female with tracheomalacia
On inspiration the trachea is normal and widely patent and on expiratation the trachea collapses to greater than 50% of its original diameter
Ashley DAvidoff MD
TheCommonVein.net
