-

Paraseptal Emphysema - Centrilobular emphysema, paraseptal emphysema, and panlobular emphysema are three different subtypes of emphysema, which is a type of chronic obstructive pulmonary disease (COPD) characterized by the destruction of the alveoli in the lungs. Each subtype has distinct features:
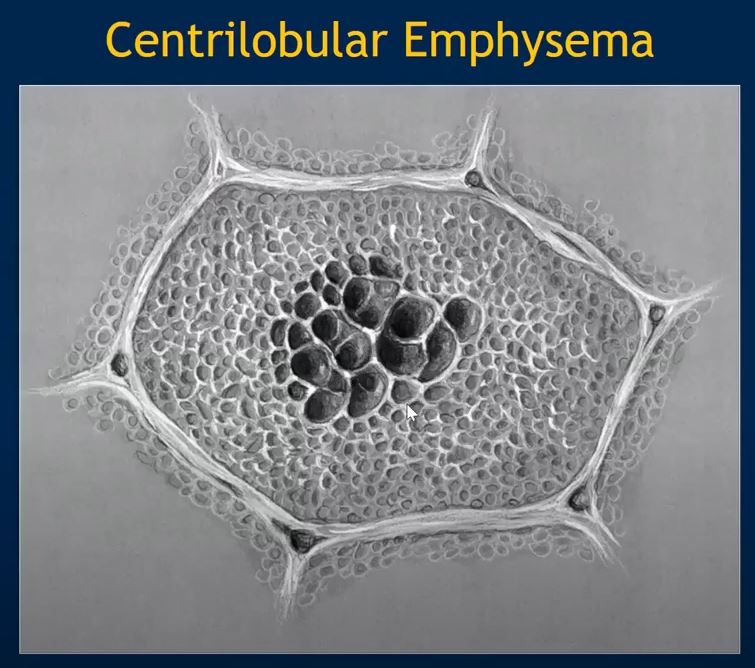
- Centrilobular Emphysema (Centriacinar Emphysema): Centrilobular emphysema is the most common form of emphysema, and it primarily affects the respiratory bronchioles within the lung’s secondary lobules. This type of emphysema is often associated with smoking. The destruction of the alveoli occurs mainly in the central or proximal parts of the secondary lobules, leaving the peripheral areas of the lobules relatively unaffected. It is often more prominent in the upper lobes of the lungs.


Emphysema
A drawing showing the normal acinus in teal and the abnormal emphysematous acinus in green characterised by destruction of the septal walls, enlargement of the alveoli, and loss of elasticity. The absence of involvement of the respiratory bronchiole makes the pathological diagnosis of centrilobular emphysema. Ashley Davidoff MD
TheCommonVein.net 32645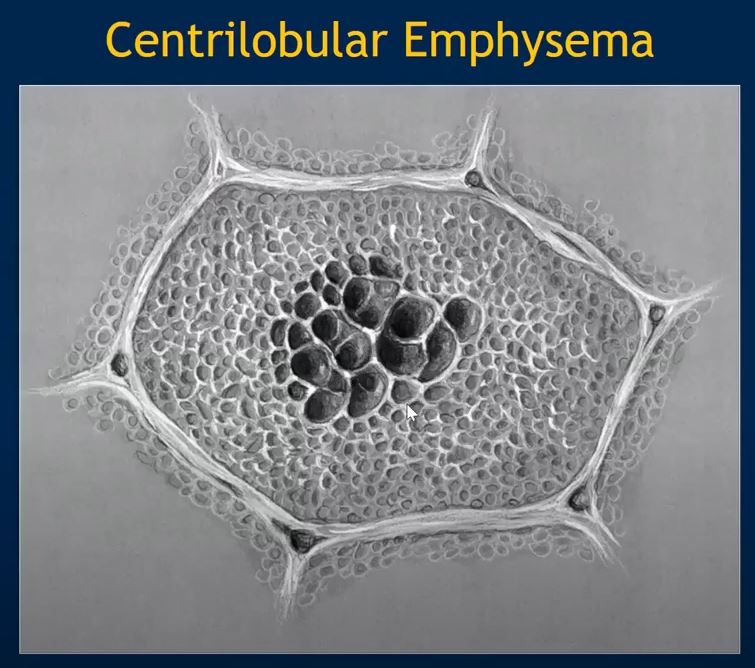
C 

Magnified view of the upper lobes of a 66year female with centrilobular emphysemashows an expanded lobule with a centrilobular vessel in the middle characteristic of centrilobular emphysema
Ashley Davidoff MD TheCommonvein.net - Paraseptal Emphysema (Distal Acinar Emphysema): Paraseptal emphysema predominantly affects the distal parts of the secondary pulmonary lobules, particularly near the pleural surfaces and interlobular septa. This type of emphysema is often seen adjacent to areas of scarring or fibrosis, and it is sometimes associated with spontaneous pneumothorax Paraseptal emphysema can occur in individuals with or without a history of smoking. Paraseptal emphysema is subpleural and peribronchovascular, interspersed with areas of intact interlobular septa.


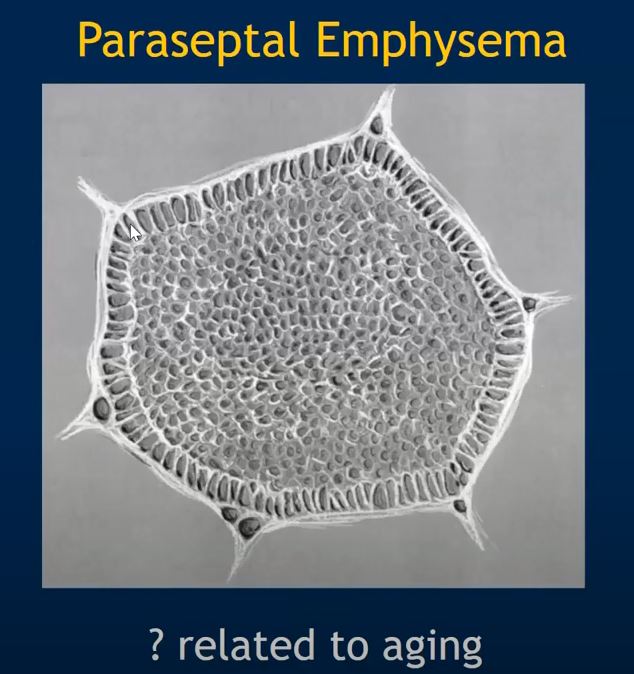
Paraseptal Emphysema Bullous emphysema can be secondary to paraseptal emphysema. Bullous emphysema is a subtype of emphysema characterized by the formation of large air spaces known as bullae within the lung tissue. These bullae can be several centimeters in diameter and are often thin-walled.

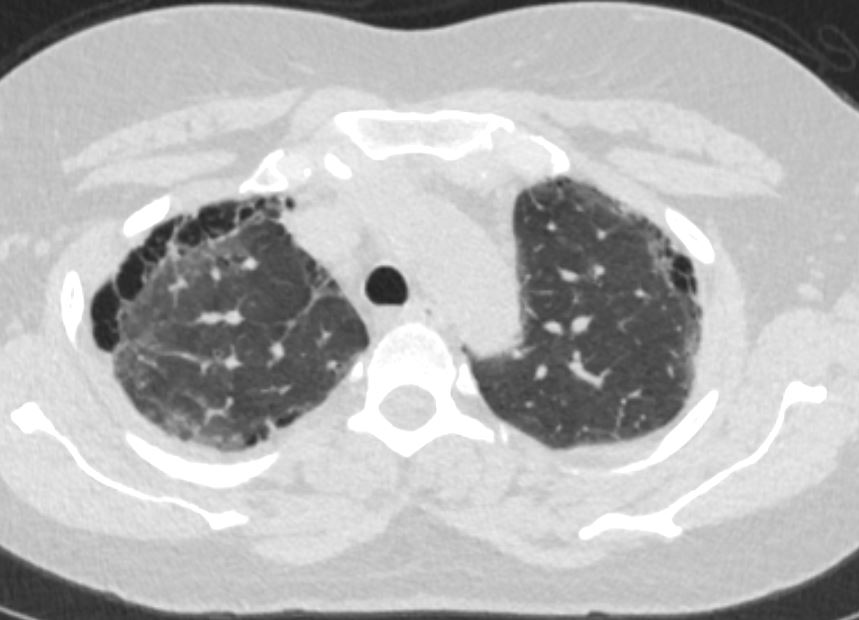
Bullous Paraseptal Emphysema with Centrilobular Emphysema
Ashley Davidoff MD
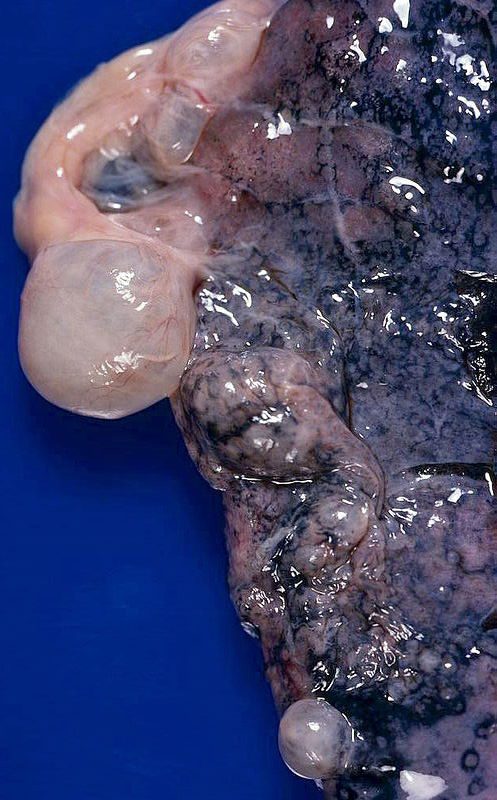
Emphysema, bullous, subpleural
Large, prominent subpleural bullae. Spontaneous pneumothorax often results from rupture of such lesions.
Bullous (paraseptal) emphysema limited to lung periphery. Usually not smoking-related. Rupture is most common cause of spontaneous penumothorax…mostly young adults.
Courtesy Yale Rosen MD(Panacinar Emphysema): Panlobular emphysema involves uniform and widespread destruction of the alveoli throughout the entire secondary pulmonary lobule. It is commonly associated with a genetic condition called alpha-1 antitrypsin deficiency, which predisposes individuals to the development of emphysema even without significant smoking history. This type of emphysema is more common in the lower lobes of the lungs.
-


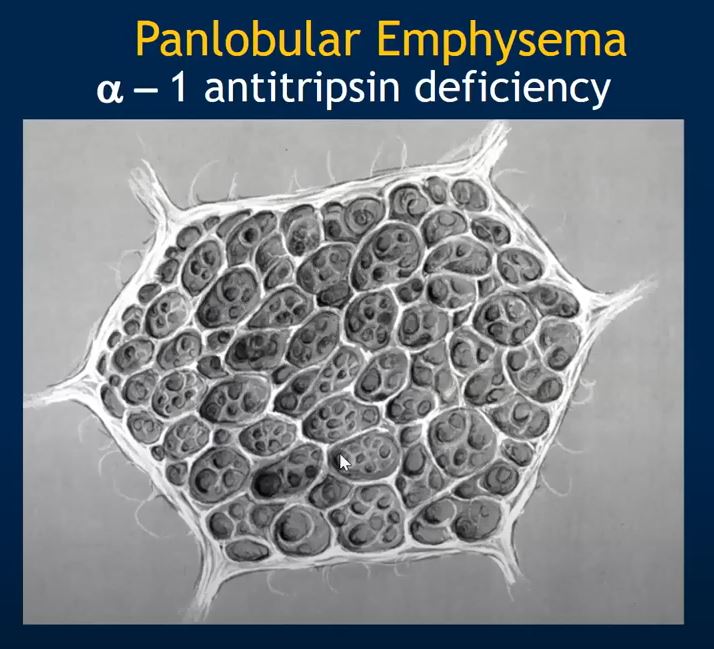
Panlobular Emphysema 

78 year old male with alph1 antitrypsin deficiency and extensive panlobular emphysema involving both the upper lobes and lower lobes
Scout film for the CT shows asymmetric hyperinflation
Ashley Davidoff TheCommonVein.net
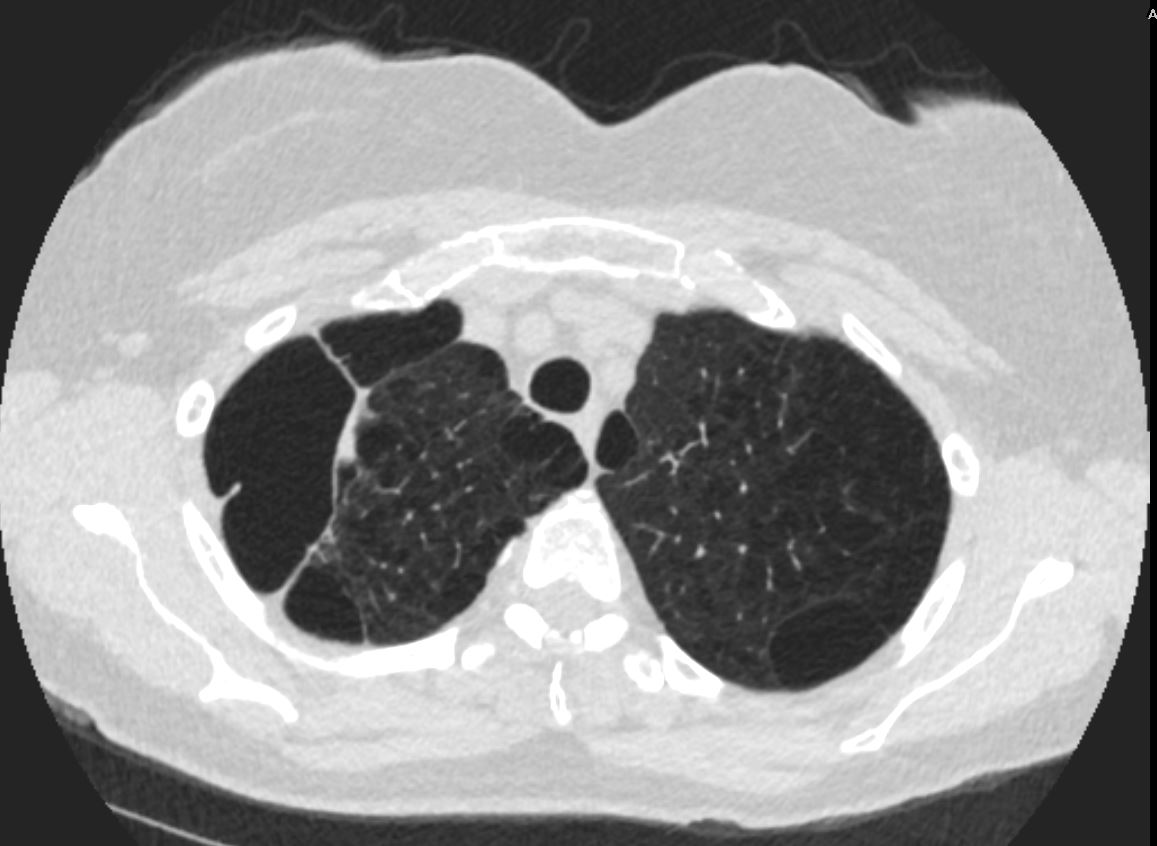
78 year old male with alph1 antitrypsin deficiency and extensive panlobular emphysema involving both the upper lobes and lower lobes
CT shows extensive severe bilateral asymmetric hyperinflation involving the upper lobes with a moderate right sided effusion with compressive atelectasis
Ashley Davidoff TheCommonVein.net

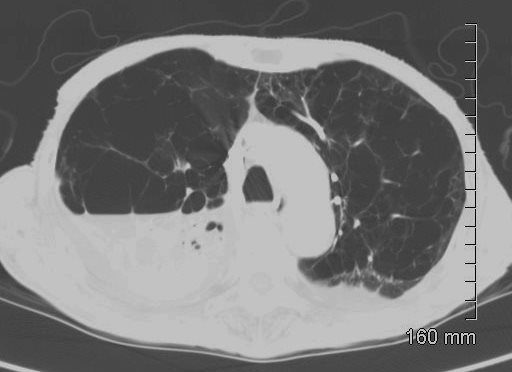
78 year old male with alph1 antitrypsin deficiency and extensive panlobular emphysema involving both the upper lobes and lower lobes
CT shows extensive severe bilateral asymmetric hyperinflation involving the upper lobes with a moderate right sided effusion with compressive atelectasis
Ashley Davidoff TheCommonVein.net
- Centrilobular Emphysema (Centriacinar Emphysema): Centrilobular emphysema is the most common form of emphysema, and it primarily affects the respiratory bronchioles within the lung’s secondary lobules. This type of emphysema is often associated with smoking. The destruction of the alveoli occurs mainly in the central or proximal parts of the secondary lobules, leaving the peripheral areas of the lobules relatively unaffected. It is often more prominent in the upper lobes of the lungs.
Shapes