- is an obstructive lung disease
- Caused by
- infection
- pneumonia
- TB aspergillosis
- smoking
- radiation therapy
- cystic fibrosis
- immune disease
- autoimmune
- HIV/AIDS
- Resulting in
- permanent enlargement of parts of the airways
- Caused by
Bronchiectasis refers to irreversible, abnormal dilation of the bronchial airways due to chronic inflammation, infection, or structural airway damage. It disrupts normal bronchial function, leading to impaired mucus clearance, recurrent infections, and airflow obstruction. A specific subtype, traction bronchiectasis, occurs due to fibrosis or scarring of the surrounding lung parenchyma, which pulls the airways open.
Radiological imaging, particularly high-resolution CT (HRCT), is critical for diagnosing and differentiating bronchiectasis subtypes, including traction bronchiectasis.
Radiological Features
- Chest X-Ray (CXR):
- Findings:
- Thickened bronchial walls visible as tram-track lines (parallel linear opacities).
- Ring shadows representing cross-sectional dilated bronchi.
- Increased lung markings or scarring in advanced cases.
- Limitations:
- CXR has low sensitivity for detecting bronchiectasis, particularly traction bronchiectasis.
- Findings:
- High-Resolution CT (HRCT):
- Gold Standard for diagnosing and characterizing bronchiectasis.
- Key Findings:
- Bronchial Dilation:
- Bronchi larger than the accompanying pulmonary arteries (signet ring sign).
- Lack of Tapering:
- Abnormal bronchi extend to the lung periphery without normal tapering.
- Bronchial Wall Thickening:
- Reflects chronic inflammation.
- Mucus Plugs:
- Internal airway opacities often seen in post-infectious or obstructive cases.
- Bronchial Dilation:
Traction Bronchiectasis (HRCT Findings)
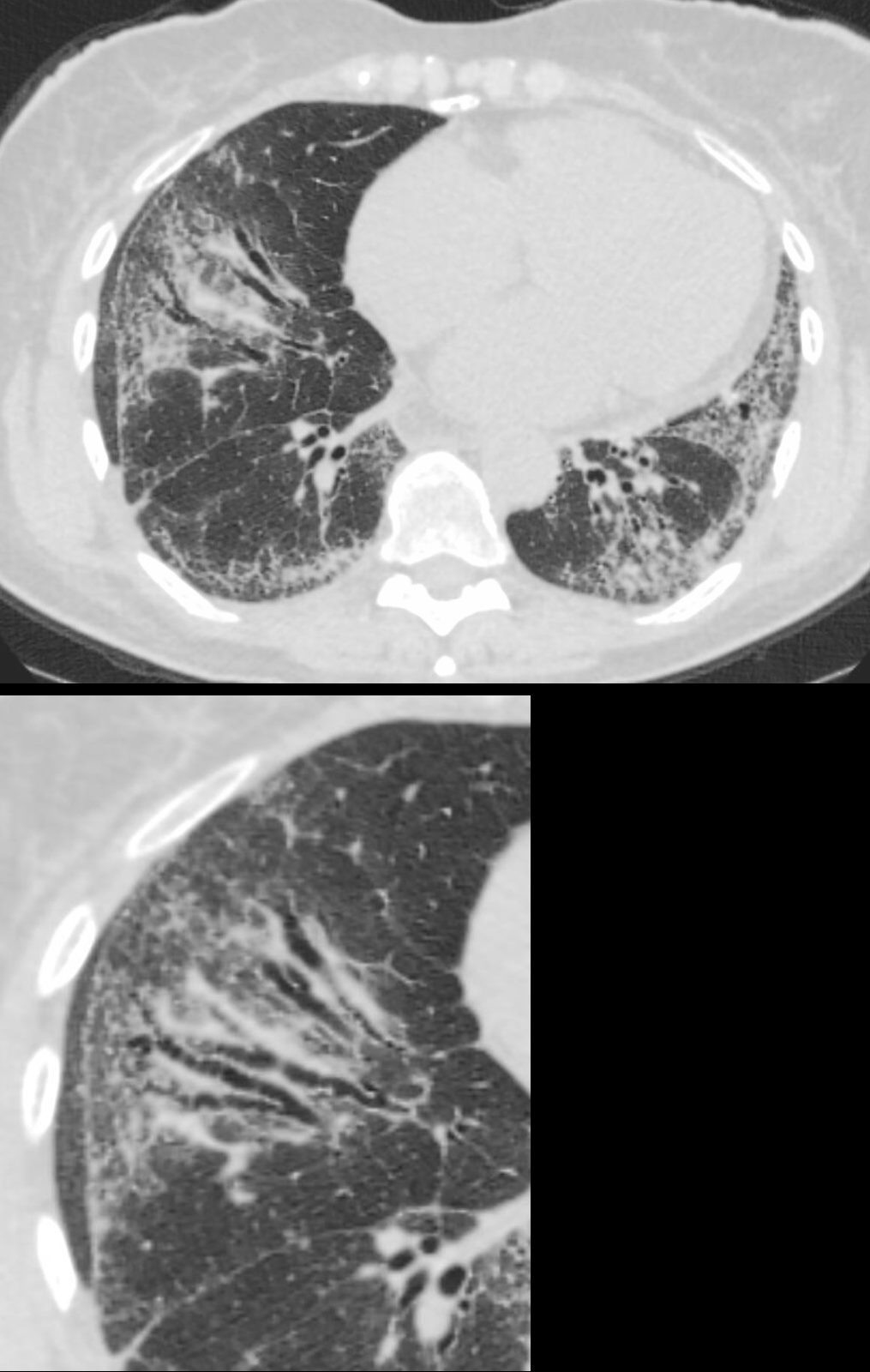
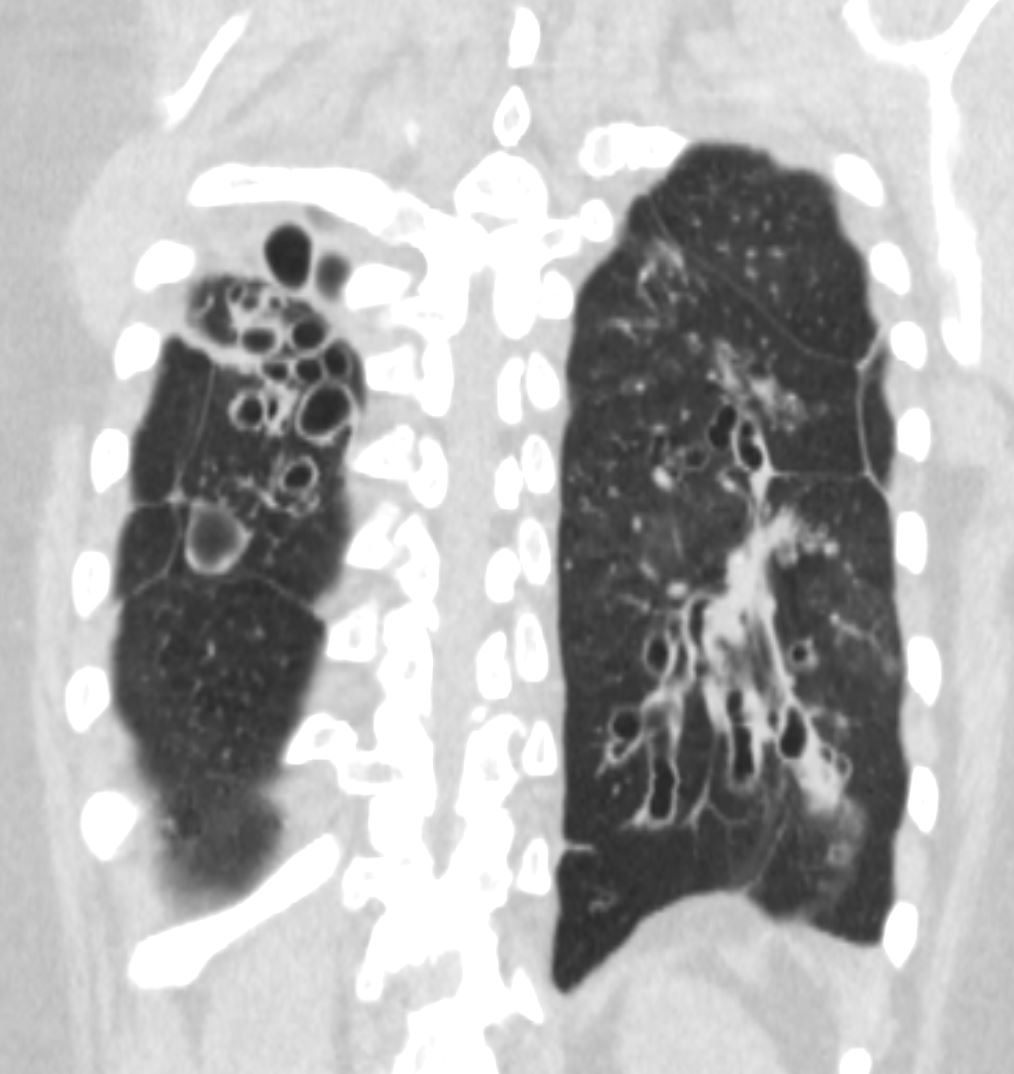
71-year-old female presents with a history of scleroderma, ILD, hypothyroidism and dcSSc
CT in the axial plane, shows extensive ground glass changes in the inferior lingula middle lobe and traction bronchiectasis in the middle lobe. The left lower lobe shows bronchovascular changes, and bronchiolectasis and there is bilateral subpleural sparing
The fissures show irregular thickening.
The lower image exemplifies the traction bronchiectasis
Ashley Davidoff MD TheCommonVein.net 196Lu 136610c
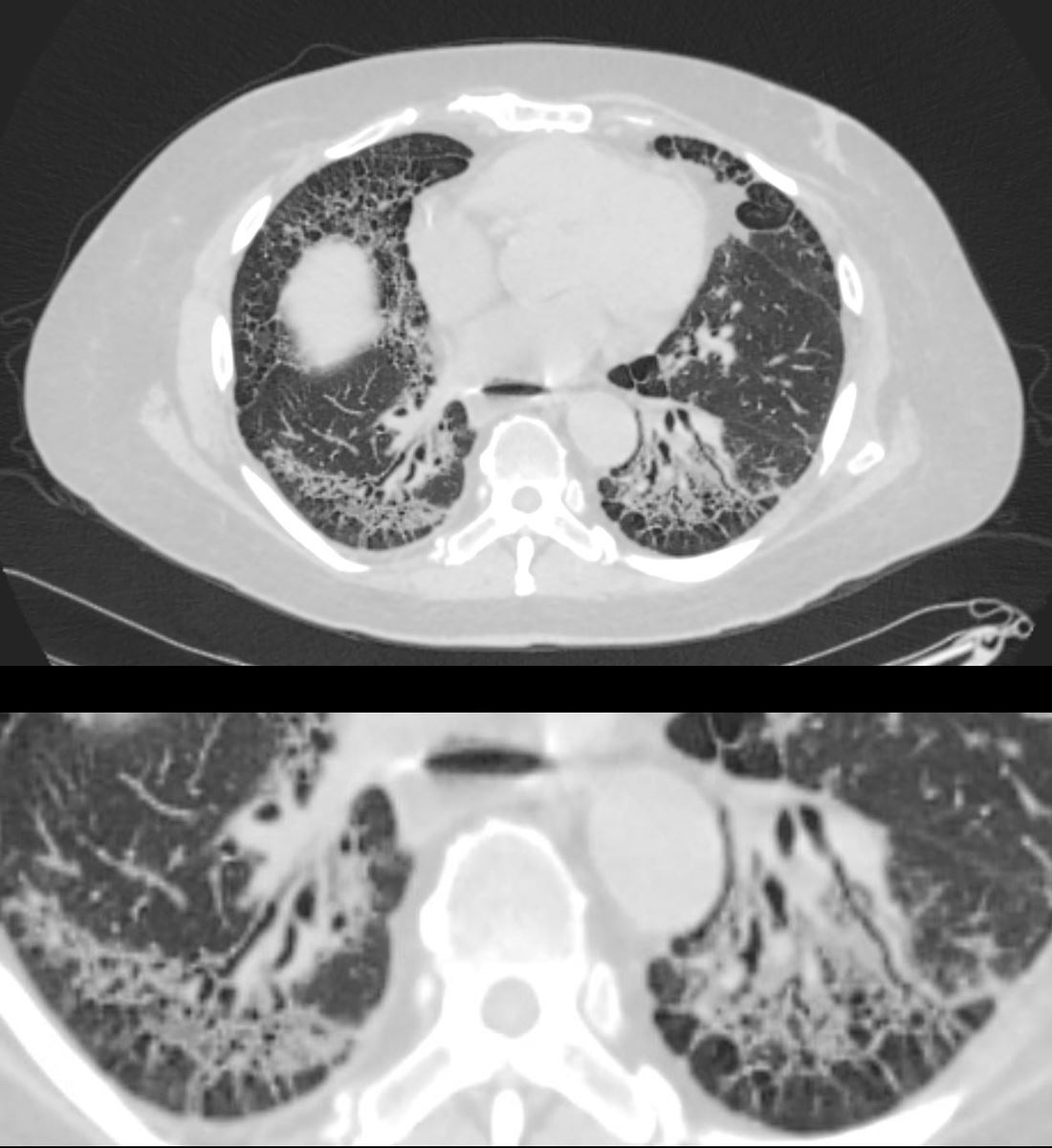
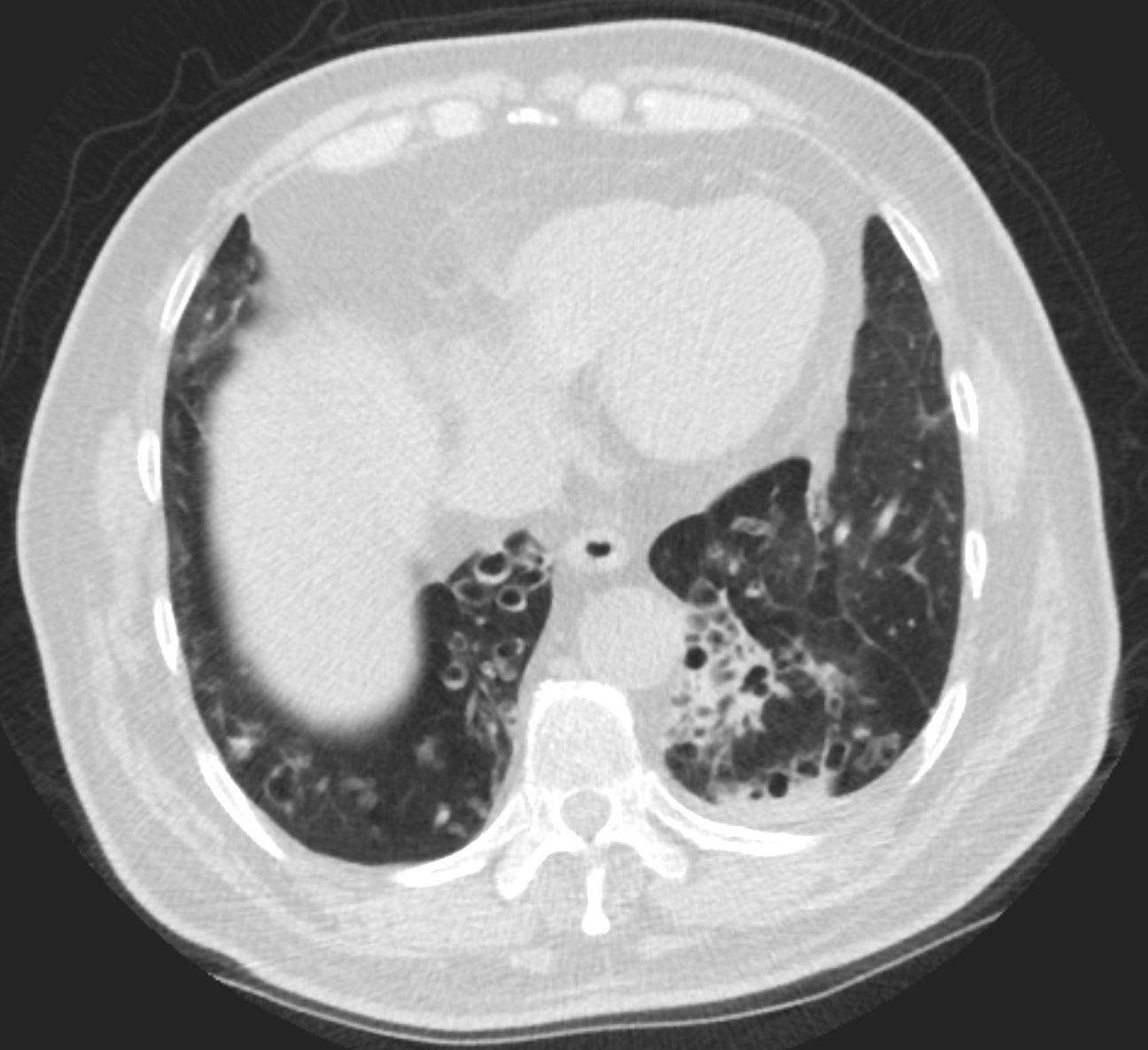
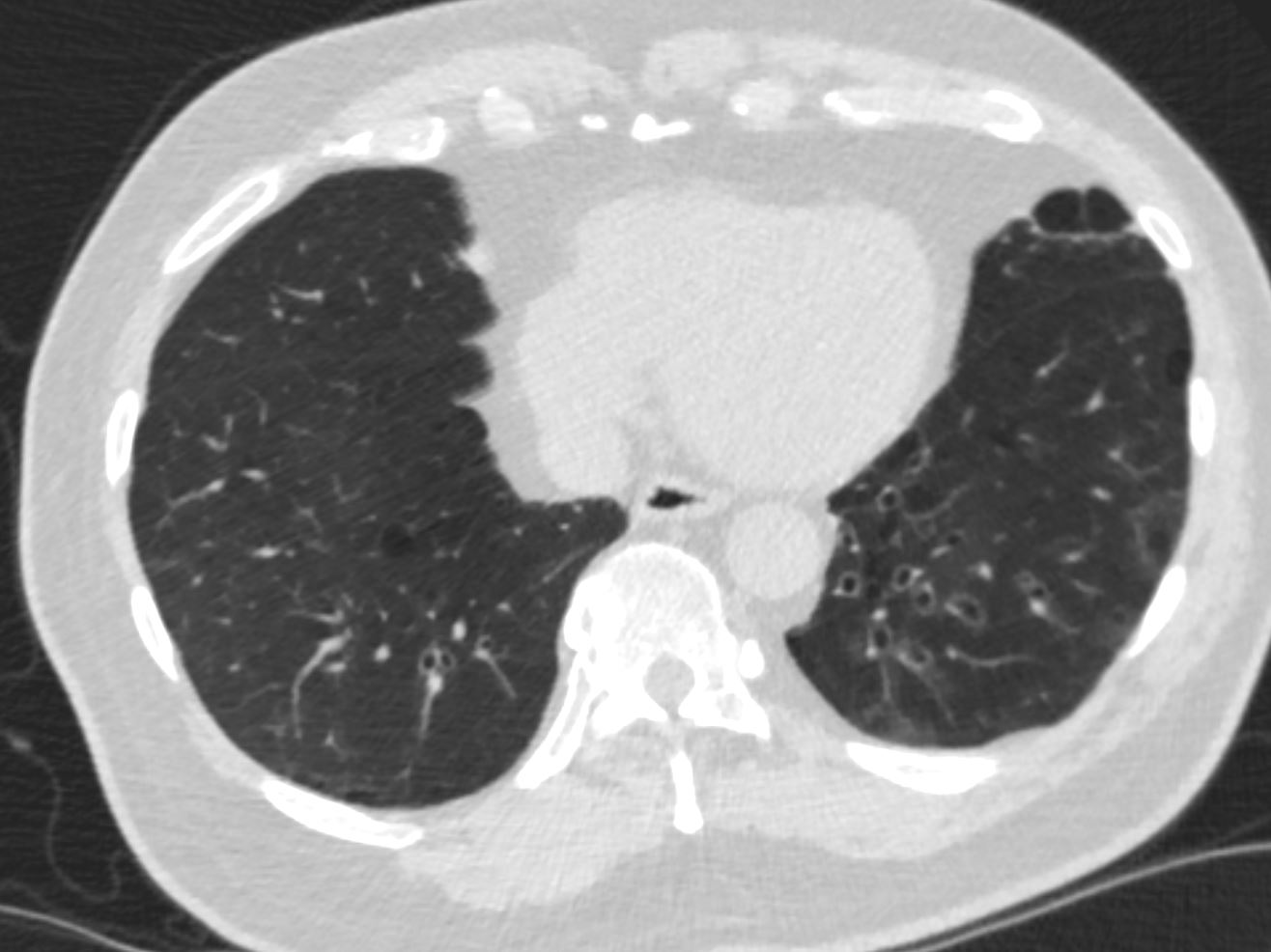
59-year-old male presents with history of scleroderma, Raynaud’s disease, and ILD
Upper Image
Axial CT shows bibasilar ground glass, bronchiectasis, and bronchiolectasis with volume loss and with crowding of the bronchovascular bundles posteriorly. There is subpleural sparing. Note air-fluid level in the distended esophagus.
The lower image focuses on the peripheral sparing. The spared secondary lobules have also undergone enlargement secondary to the fibrotic process
Ashley Davidoff MD TheCommonVein.net 110Lu 136598c01
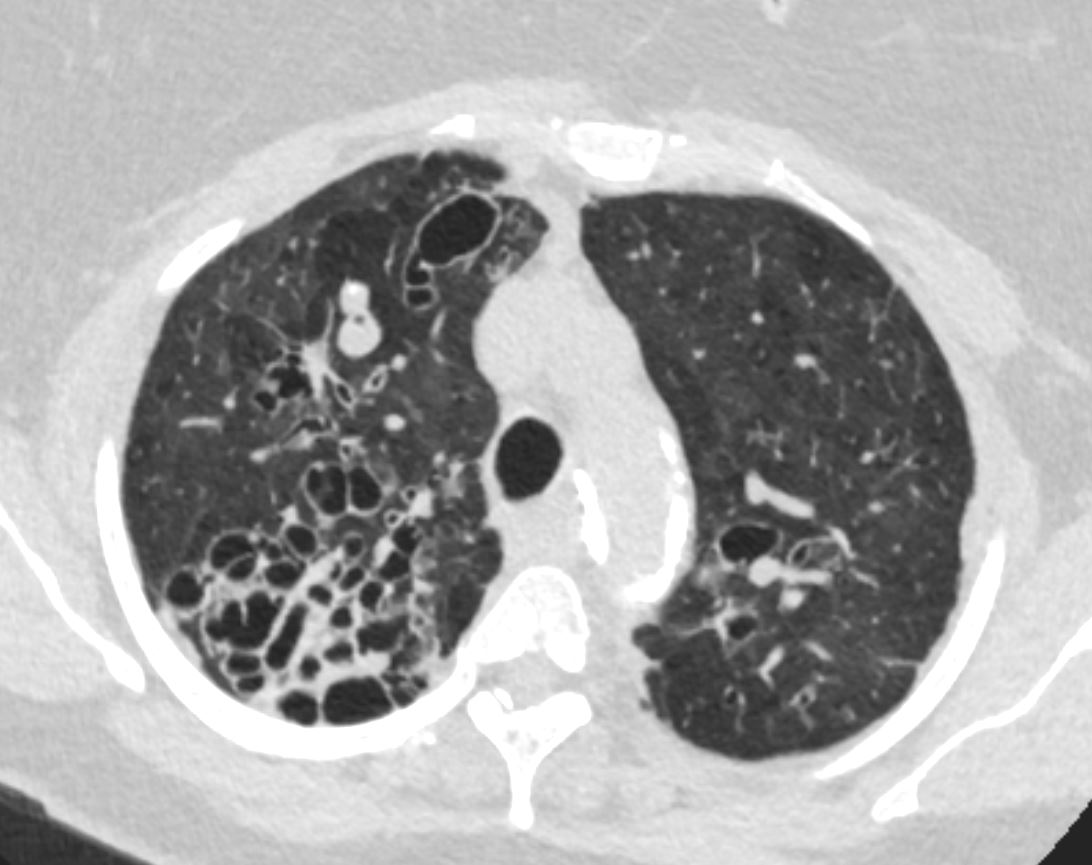
Chronic MAC Infection
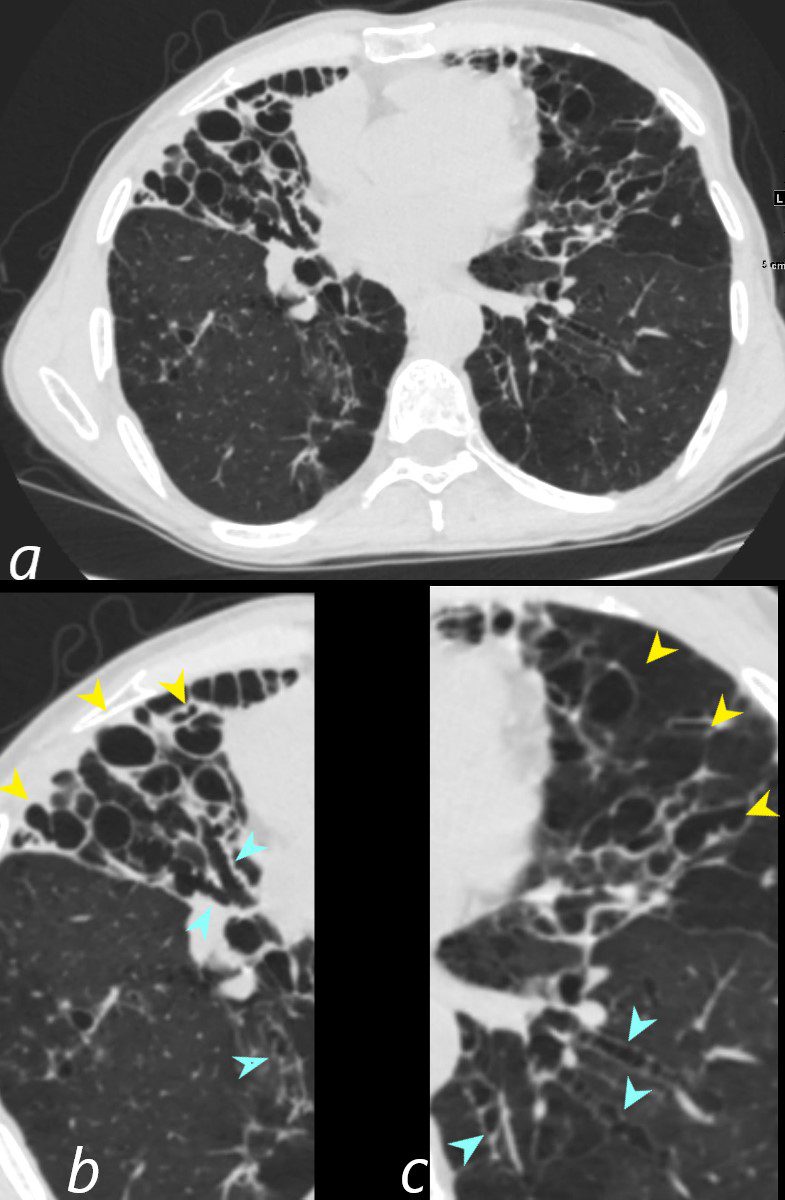
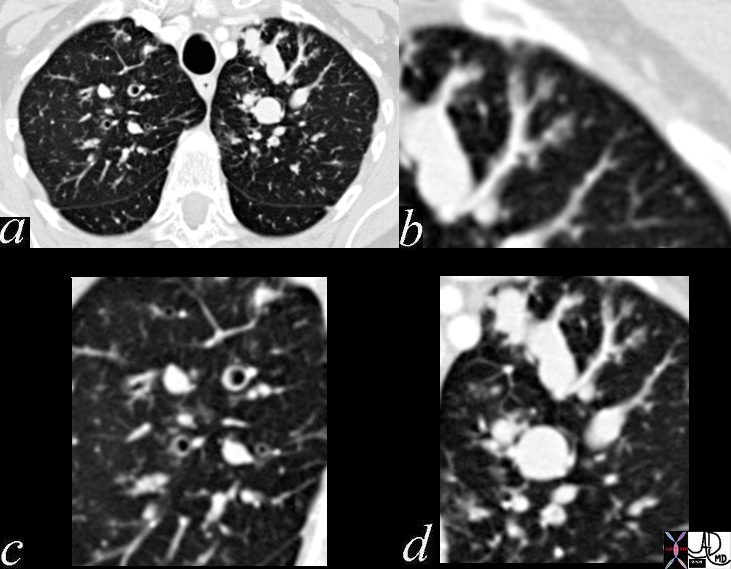
61-year-old male with a history of treated mycobacterial infections including MAC and chronic cough.
Axial CT at the level of the mid to lower chest shows mildly ectatic segmental airways to the lower, and middle lobe bronchi but significant bronchiectasis to the middle lobe and lingula involving the subsegmental airways. There is a relative paucity of mucus in the ectatic airways. The history of MAC and the distribution of the bronchiectasis in the middle lobe and lingula are reminiscent of the diagnosis of Lady Windermere syndrome
Ashley Davidoff MD TheCommonVein.net 250Lu 135876
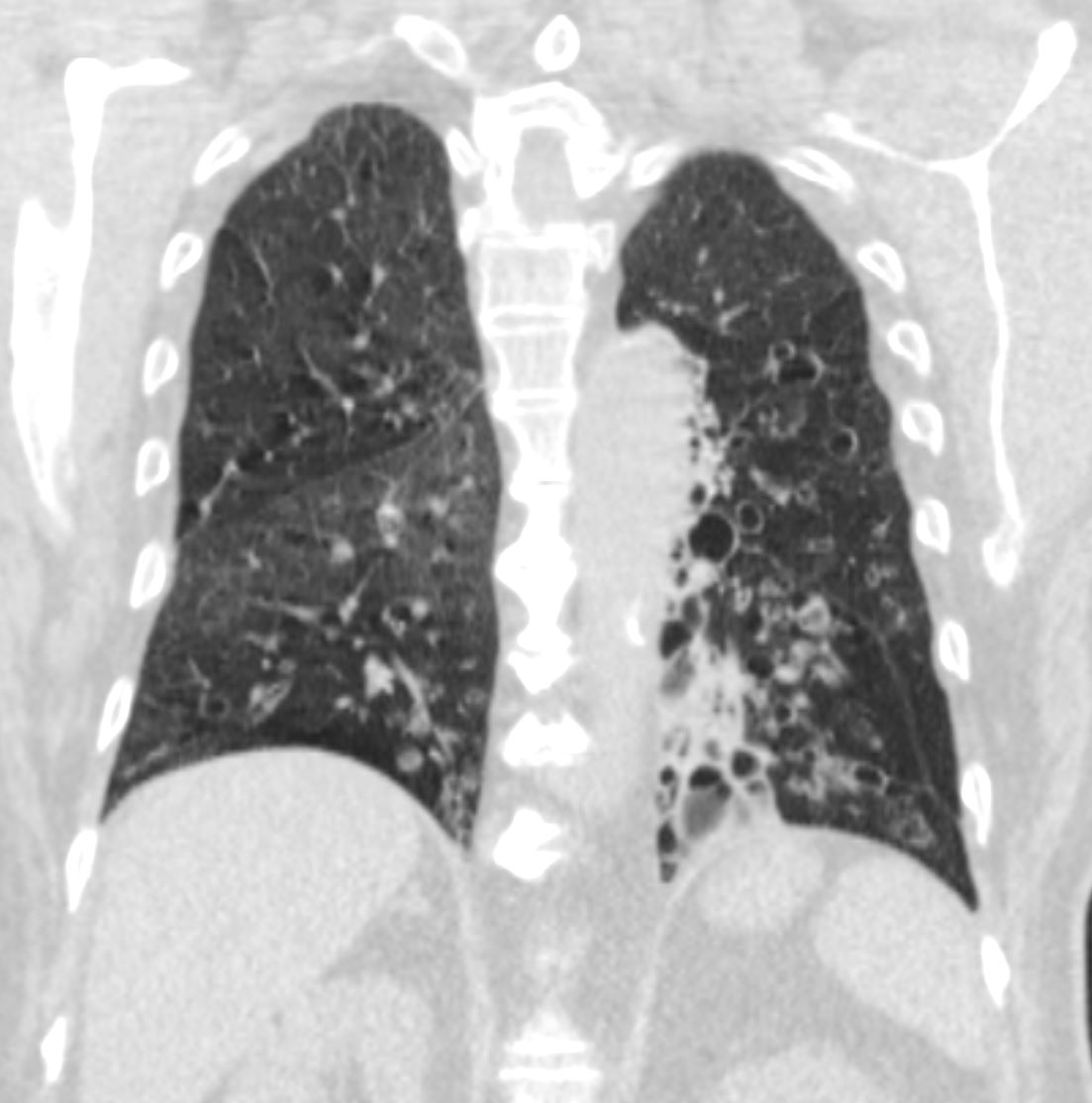
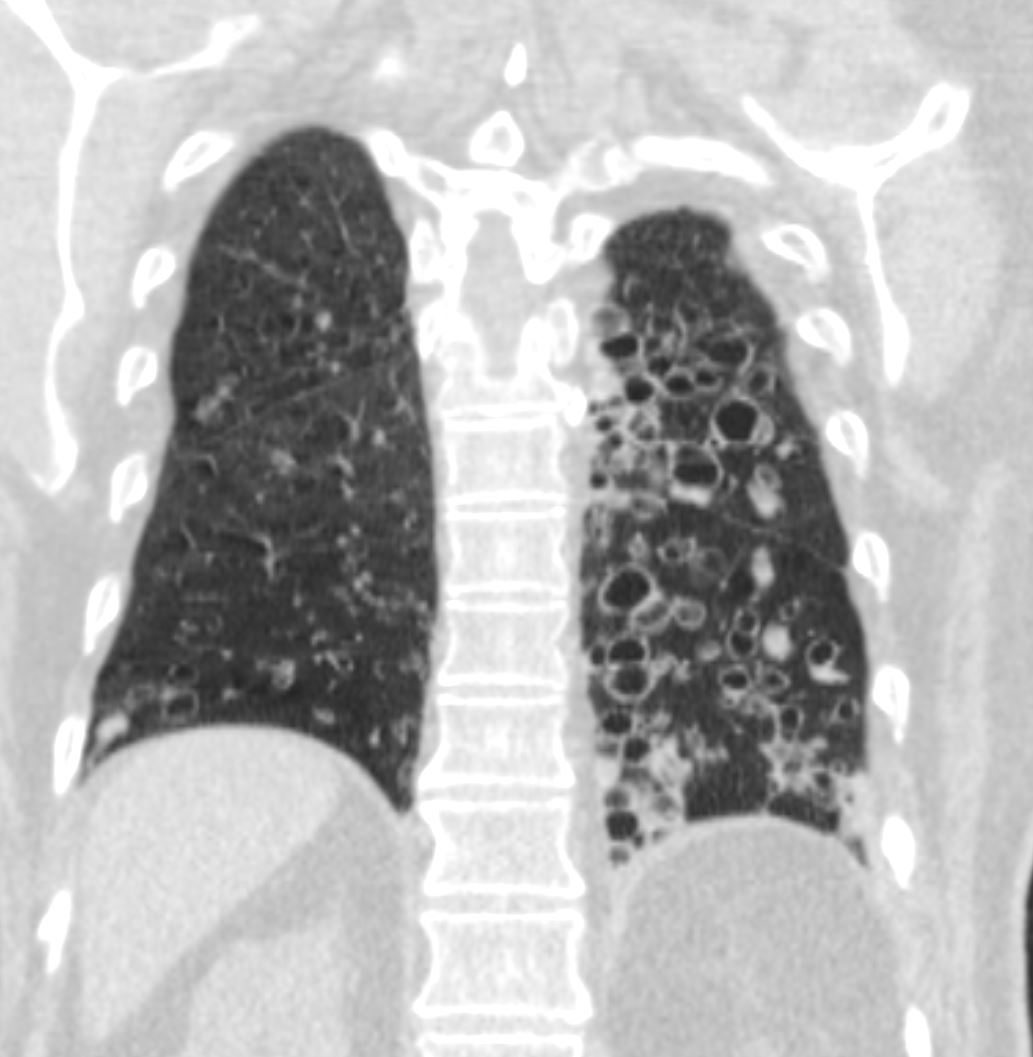
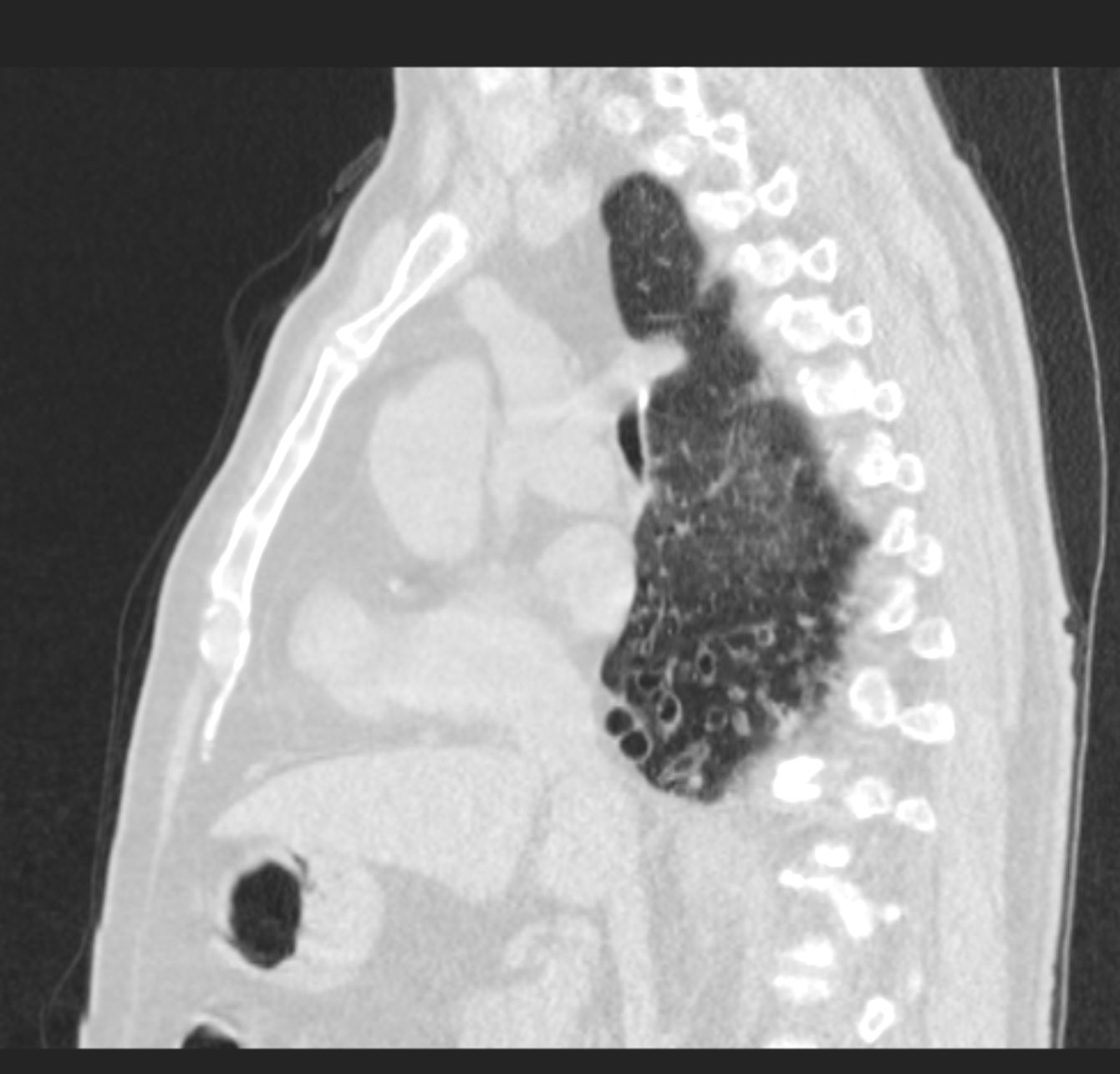
Cystic Bronchiectasis and Cicatricial Atelectasis
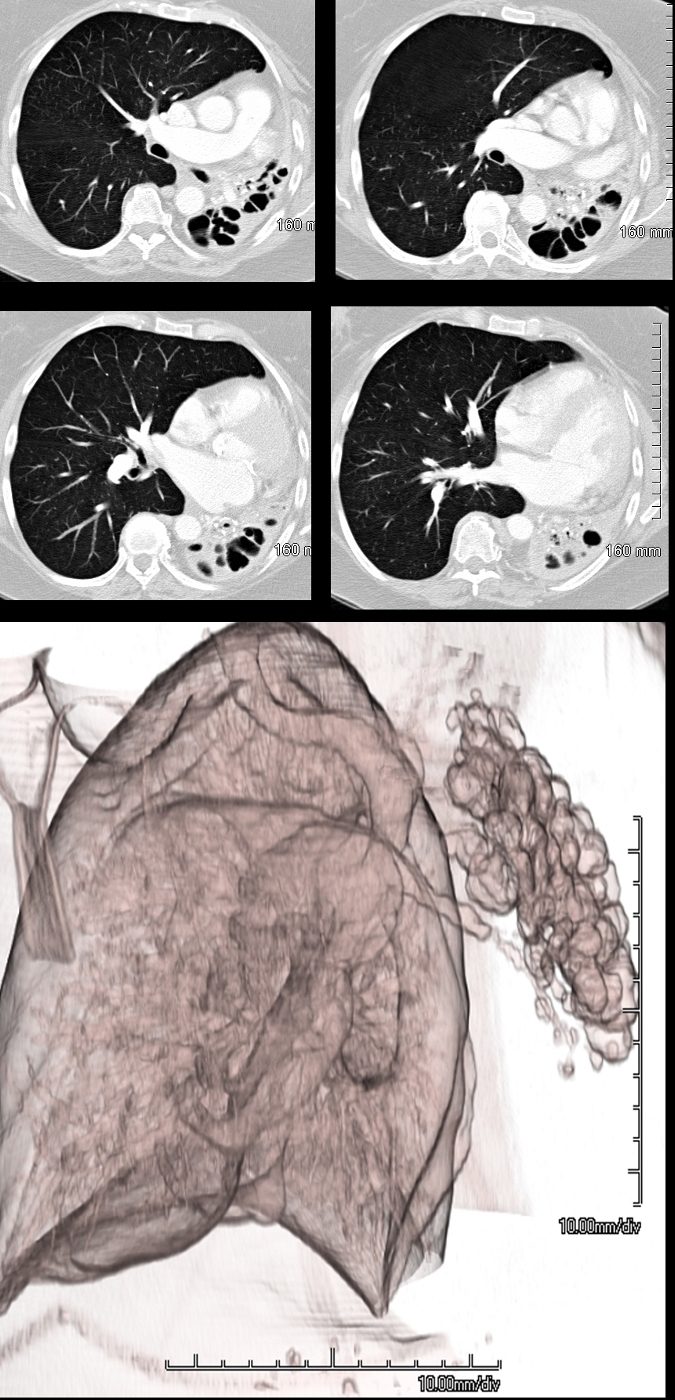
69 year female atrophied left lung secondary to chronic infection and resulting in cystic bronchiectasis (aka saccular bronchiectasis)
The axial images show a totally collapsed left lung with leftward mediastinal shift and hyperinflation of the right lung. The airways of the left lung are large and patent allowing for a 3Dreconstruction of the airways and confirming the diagnosis of saccular bronchiectasis. The atelectasis of the left lung is called cicatricial atelectasis secondary to chronic fibrosis
Ashley Davidoff MD TheCommonvein.net 117955c
-
- Cause:
- Secondary to fibrotic processes that exert pulling forces on the airways, leading to dilation.
- Associated Conditions:
- Interstitial lung diseases (ILD):
- Especially idiopathic pulmonary fibrosis (IPF), sarcoidosis, or chronic hypersensitivity pneumonitis.
- Radiation-induced fibrosis or post-inflammatory scarring.
- Interstitial lung diseases (ILD):
- Imaging Features:
- Irregularly dilated bronchi located in regions of fibrotic changes.
- Often associated with honeycombing, ground-glass opacities, or architectural distortion.
- Peripherally distributed in fibrotic diseases, often near subpleural regions.
- Cause:
- MRI:
- Rarely used but can evaluate bronchiectasis and mucus plugging, especially in cystic fibrosis patients.
Classification
- Morphological Types (on HRCT):
- Cylindrical:
- Uniformly dilated bronchi resembling tubes; common in post-infectious bronchiectasis.
- Varicose:
- Irregularly dilated bronchi with alternating areas of dilation and narrowing; seen in chronic infections.
- Cystic (Saccular):
- Severely dilated bronchi forming cyst-like structures, associated with advanced disease.
- Traction:
- Bronchiectasis caused by fibrotic retraction of surrounding lung tissue.
- Cylindrical:
- Distribution:
- Localized:
- Limited to one lobe or segment (e.g., post-obstructive bronchiectasis).
- Diffuse:
- Involves multiple lobes, often seen in systemic diseases or infections (e.g., cystic fibrosis, ILD).
- Localized:
Causes and Associations
- Post-Infectious:
- Common in tuberculosis, pertussis, measles, or necrotizing bacterial infections.
- Interstitial Lung Diseases (Traction Bronchiectasis):
- Idiopathic Pulmonary Fibrosis (IPF):
- Classically associated with subpleural honeycombing and traction bronchiectasis.
- Sarcoidosis:
- Granulomatous inflammation leading to fibrosis and airway distortion.
- Chronic Hypersensitivity Pneumonitis:
- Causes peripheral fibrosis with traction bronchiectasis.
- Idiopathic Pulmonary Fibrosis (IPF):
- Cystic Fibrosis:
- Common cause of diffuse bronchiectasis.
- Obstructive:
- Airway obstruction from foreign bodies, tumors, or mucus plugging.
- Congenital Disorders:
- Kartagener’s syndrome (primary ciliary dyskinesia), Williams-Campbell syndrome.
Complications
- Recurrent Infections:
- Leads to progressive lung damage.
- Hemoptysis:
- Due to erosion of bronchial blood vessels.
- Respiratory Failure:
- Advanced disease with airflow obstruction.
- Pulmonary Hypertension:
- Rare, due to chronic hypoxia.
Clinical Relevance
Including traction bronchiectasis highlights the importance of recognizing fibrotic processes that distort airway anatomy. Identifying the pattern and distribution of bronchiectasis (e.g., traction vs. inflammatory) on imaging is essential for targeting treatment and evaluating prognosis.
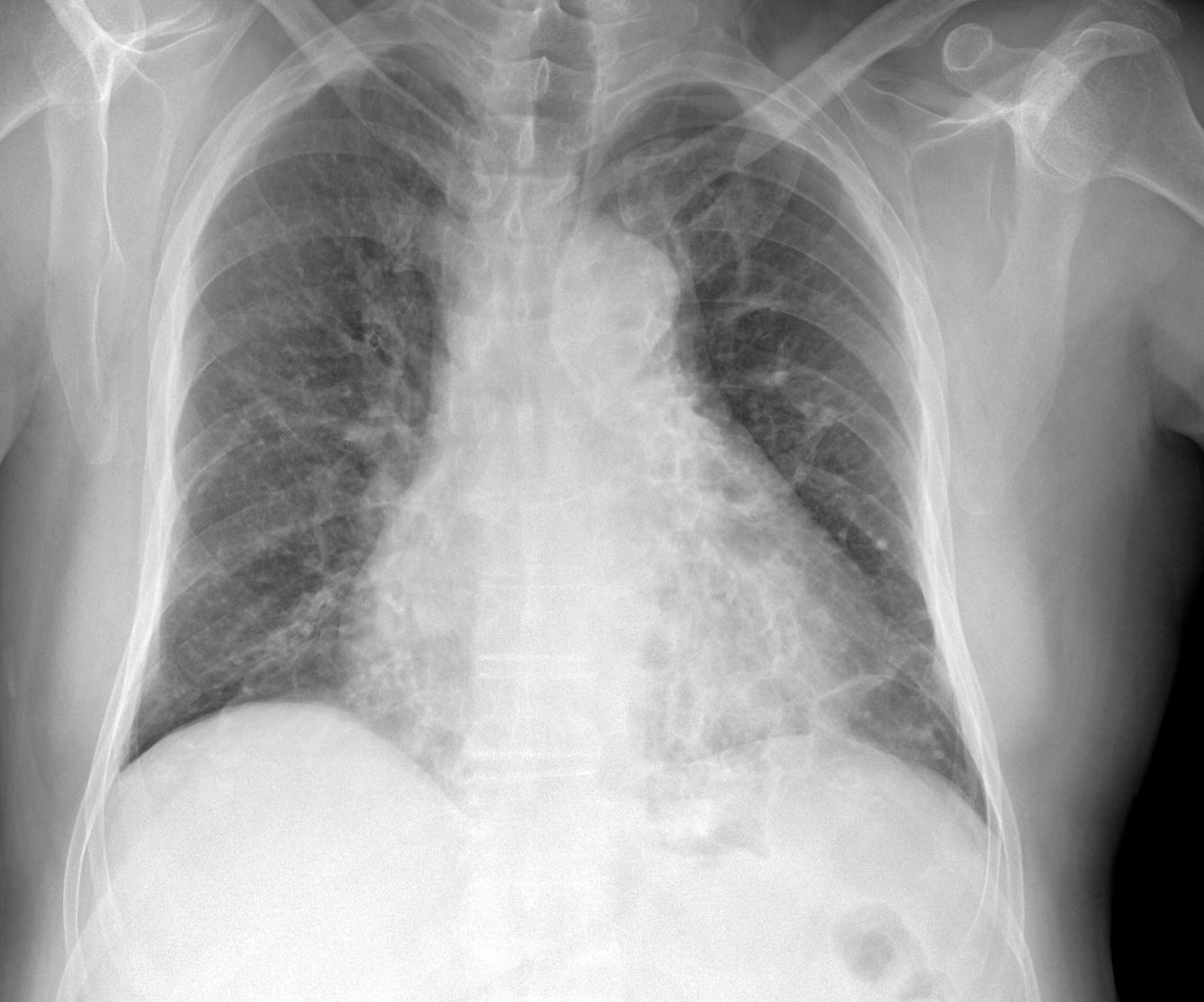
Apical Bronchiectasis – Possibly TB

CT scan through the apex of the lungs of a 100 year old female showing evidence of bilateral apical bronchiectasis (top) with correlative plain film findings in the plain film (below) The most common cause is TB. The MPA is enlarged consistent with the diagnosis of pulmonary hypertension.
Ashley Davidoff MD
- Emphysema
- Smoking and Bronchiectasis –
-
- Loss of ciliary function by cigarette smoke
- Increase mucus production with decrease clearing
- Increase infection
-
Saccular Bronchiectasis

Ashley Davidoff MD TheCommonVein Bronchiectasis 001
Ashley Davidoff
TheCommonVein.net

Ashley Davidoff
TheCommonVein.net
Ashley Davidoff
TheCommonVein.net
Ashley Davidoff
TheCommonVein.net
Ashley Davidoff
TheCommonVein.net
Ashley Davidoff
TheCommonVein.net

Ashley Davidoff
TheCommonVein.net
Mucus Filled airway with Distal Hyperinflation

Ashley Davidoff MD TheCommonVein.net bronchiectasis 006b
Ashley Davidoff MD TheCommonVein.net bronchiectasis 005
Ashley Davidoff MD TheCommonVein.net bronchiectasis 006
Bronchiectasis and Atelectasis
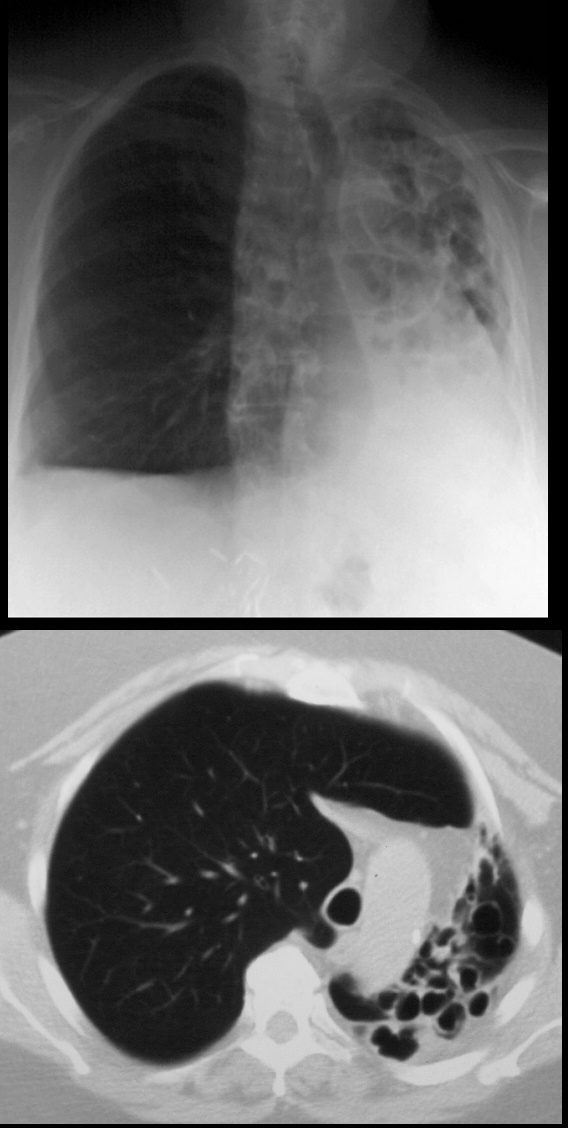
68year old male presents with chronic cough. Chest Xray reveals evidence of tram tracking and bronchiectasis in the left lung with volume loss of the entire right lung with secondary hyperinflation of the right lung, and mediastinal shift. CT scan shows severe volume loss and hyperinflation of the right lung.
Ashley Davidoff MD TheCommonVein.net
CT scan through the chest shows medium sized bronchi, bronchioles and small airways impacted with fluid. This collage is presented to reveal tree in bud changes resulting from impaction in the smaller terminal bronchioles and respiratory units. The tree-in-bud pattern also results in small centrilobular nodules connected to multiple branching linear structures of similar caliber from a single stalk. Originally it was felt to result from endobronchial spread of Mycobacterium tuberculosis, but is is now recognized in diverse entities including peripheral airway diseases caused by infection (bacterial, fungal, viral, or parasitic), congenital disorders, idiopathic disorders (obliterative bronchiolitis, pan bronchiolitis), aspiration or inhalation of foreign substances, immunologic disorders, connective tissue disorders and peripheral pulmonary vascular diseases such as neoplastic pulmonary emboli.
In this case there are also dilated medium sized airways, impacted with soft tissue characteristic of the finger in glove sign and most likely due to allergic bronchopulmonary aspergillosis (ABPA)
Ashley Davidoff MD Ashley Davidoff MD TheCommonVein.net
47113c01
Compare the two Sides
Compare the 2 bases
Ashley Davidoff MD TheCommonVein.net
Links and References
Milliron B, et al Bronchiectasis: Mechanisms and Imaging Clues of Associated Common and Uncommon Diseases RadioGraphicsVol. 35, No. 4 2015
- TCV
- Bronchiectasis
- 032Lu Bronchiectasis and Emphysema
- 034Lu Basal Bronchitis Bronchiectasis Young Female
- 044Lu Chronic Inactive TB Lymphatic Distribution
- 003MC Kartagener’s and Bronchiectasis
- 054 LU Right Middle Lobe Syndrome – Bronchiectasis probable TB
- 063LU Sarcoidosis and Bronchiectasis
- 72LU TB and Bronchiectasis
- 73Lu TB Bronchiectasis
- Bronchiectasis
Kartagener’s syndrome TCV page
Fleischner Society
Pathology.—Bronchiectasis is irreversible localized or diffuse bronchial dilatation, usually resulting from chronic infection, proximal airway obstruction, or congenital bronchial abnormality (,26). (See also traction bronchiectasis.)
Radiographs and CT scans.—Morphologic criteria on thin-section CT scans include bronchial dilatation with respect to the accompanying pulmonary artery (signet ring sign), lack of tapering of bronchi, and identification of bronchi within 1 cm of the pleural surface (,27) (,Fig 11). Bronchiectasis may be classified as cylindric, varicose, or cystic, depending on the appearance of the affected bronchi. It is often accompanied by bronchial wall thickening, mucoid impaction, and small-airways abnormalities (,27–,29). (See also signet ring sign.)
