Introduction
Imaging is essential to the diagnosis and staging of lung cancer and therefore intimately related to the treatment. The advances made in imaging over the last two decades have radically changed the diagnostic approach to cancer. Although chest X-ray is an important study, in the face of the new technology it lags significantly in sensitivity and specificity.
High resolution CT has enabled the detection of very small nodules but in view of the lack of specificity, many unnecessary scans were being performed for small indeterminate nodules at great cost and with unnecessary radiation in the hope that a two year follow up would be able to distinguish between benign and malignant disease. The protocol for these indeterminate nodules has now been revised now that adequate data has accumulated ((McMahon).
As a result of the identification of small ground glass opacity lesions by CT, understanding of the connection and implications of premalignant atypical adenomatous hyperplasia, BAC, (carcinoma in situ)and adenocarcinoma is evolving. (Travis)
PET scanning and specifically PET-CT has been a major advance in the characterization of lesions > 7mm and now an integral and essential part of staging.
CXR
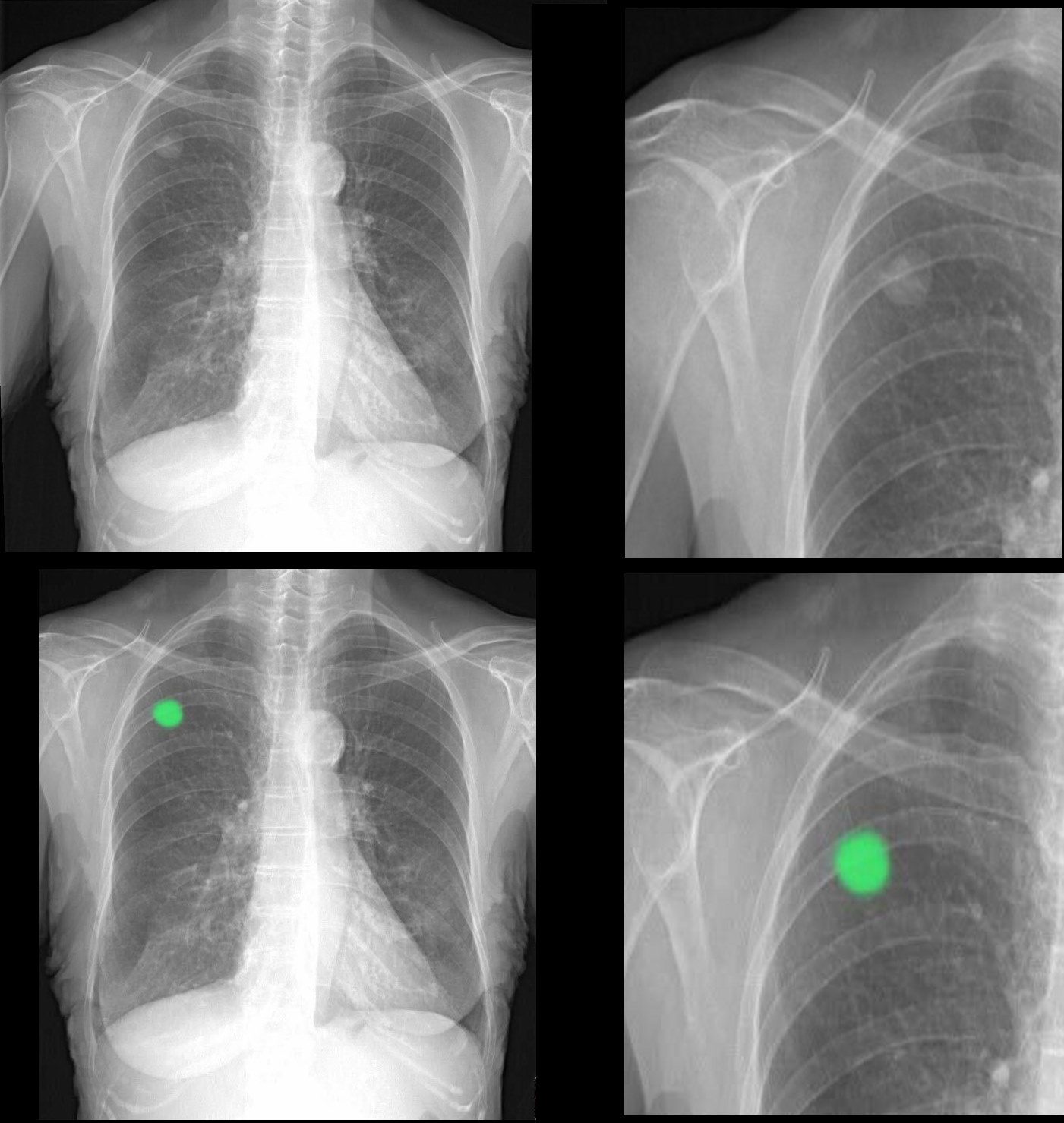
The chest X-ray often uncovers the asymptomatic nodule, but on the other hand in general has a relatively low sensitivity for identifying lung nodules and mediastinal disease. Attention to the lateral examination is important because posterior and medial lesions as well as retrocardiac lesions are often hidden in the PA exam and will be identified by the experienced radiologist on the lateral examination. If a chest x-ray is normal in a patient with high clinical suspicion, CT scan is recommended.
Atelectasis that does not resolve with time should also raise suspicion for a proximal obstructing lesion and requires further evaluation with bronchoscopy and CT scan.
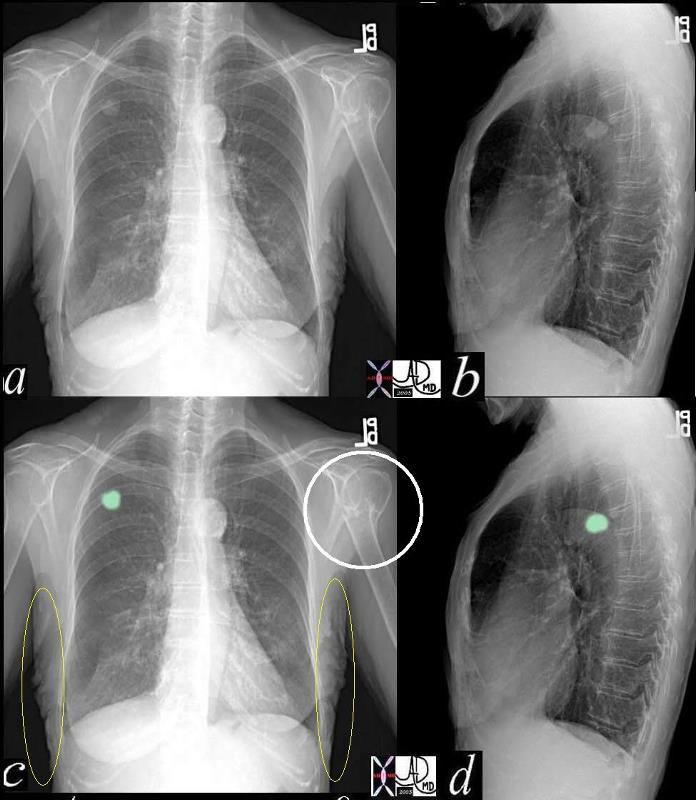
In this instance a well defined nodule is noted in the right upper lobe without other obvious adenopathy. There is a fracture of the right humerus (white ring in c) which may be due to minor trauma in this osteoporotic elderly female though a metastatic lesion to the bone is included as a possibility. The lungs are hyper inflated characterized by flattened hemi diaphragms and increase in the retrosternal space suggesting emphysema. The lesion was subsequently shown to be carcinoma
Ashley Davidoff MD
TheCommonVein.net
42263c03
The CXR is limited and a CT needs to be performed to further characterize the lesion and define the extent of the disease.
Computerized Tomography (CT/CAT)
Lung lesions with an irregular spiculated border and a diameter > 3 cm should be regarded as highly suspicious for malignancy. It is however important to maintain a high level of suspicion for all lung nodules that do not contain central calcification, particularly in smokers and patients with COPD.
Small (<5mm) smooth nodules in low risk patients are being viewed with less suspicion and 99% of such nodules are benign. (McMahon)
If there has been no change in the size of an indeterminate nodule on serial chest CT scans over a period of 2 or more years, then the lesion can be considered benign. The exception is the ground glass opacity (GGO) which if it represents BAC, may be sufficiently slow growing to show no change in 2 years.
Bronchioloalveolar carcinoma presents as ground glass opacities (GGO) either single and focal or multiple, or as an infiltrate.
The distinction between peripheral and central masses is better evaluated by axial imaging, and CT is also more sensitive to subtle calcification and cavitation of squamous malignancy.
Enhancement of a solitary pulmonary nodule by more than 20 HU following intravenous contrast is a good predictor of malignancy.(Swensen)
A lung lesion that is < 3cm in size, with well-defined margins and high attenuation values >164 suggesting that it contains calcium is considered benign.
Ashley Davidoff
The CommonVein.net

Ashley Davidoff
The CommonVein.net

Ashley Davidoff MD
TheCommonVein.net
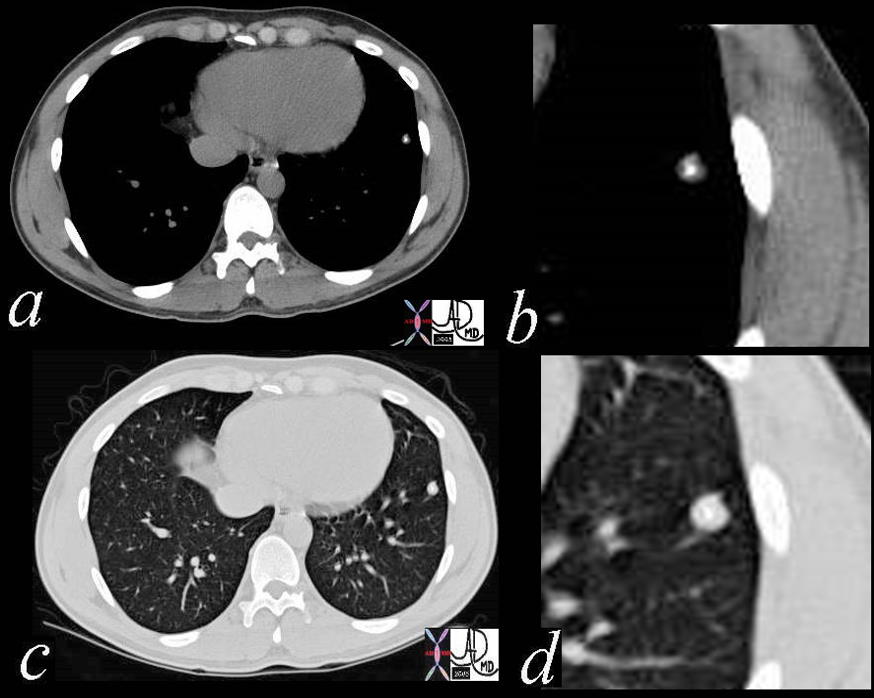
Central Cavitating Lesion
Axial CTscan through the chest in 53 year old male shows a central 2.9cms cavitating lesion consistent with a squamous cell carcinoma of the lung.
Courtesy Ashley Davidoff MD
TheCommonVein.net
87739c.8s
Central Obstructing Lesion
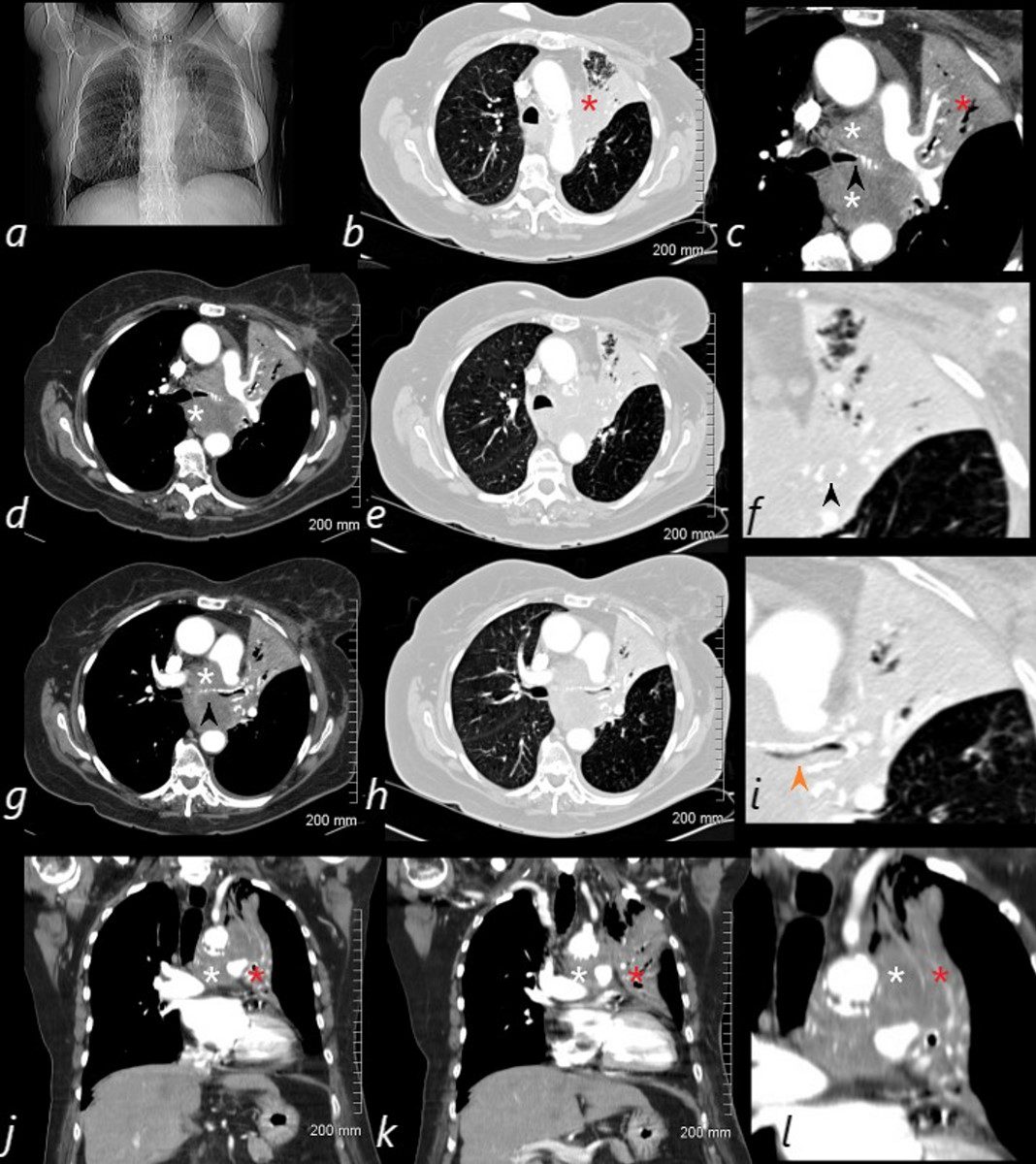
82-year-old female with dyspnea presents with an obstructing lesion of the left main stem bronchus and total atelectasis of the left lung caused by a central squamous cell carcinoma mass. The scout film (a) shows a vague area of increase density in the left upper lung field, with minimal elevation of the left mainstem bronchus. The central mass (white asterisk – is noted in c, d, g, j, k and l. Invasion and obstruction of the left main stem bronchus (black arrow – f, g) with invasion into the lumen without obstruction is notes in I – orange arrow. Post obstructive atelectasis of the left upper lobe is noted (red asterisk – b,c,j,k,l) with hyperinflated left lower lobe extending to the left apex.
Ashley Davidoff MD TheCommonVein.net
PET scanning and specifically PET-CT has been a major advance in the characterization of lesions. It is true functional imaging and reflects the metabolic activity of a nodule or mass in question. Tumor cells are typically metabolically active and hence will take up more glucose than most normal cells.
The PET tracer (usually FDG) consists of two parts; glucose and a radioactive component. The most widely used compound is a glucose analogue 18F-fluoro-2deoxy-D glucose which becomes trapped inside tumor cells which use the glucose in metabolism. In general the patient is scanned about 45-60 minutes after the compound is administered intravenously. The emitted positrons from the radioactive component can be detected by a scanner and is reflected as a 3D image.
Because PET scanning measures functional changes it will reflect changes in biologic activity before structural changes are apparent. Thus changes in management can be made earlier as result of functional evaluation.
The combined use of PET and CT allows for combined structural and functional imaging In essence FDG activity is overlaid on the CTscan which will allow accurate structural localization.
FDG is normally distributed in the brain, heart, stomach, kidneys, and bladder.
In the sphere of lung cancer PET is used to differentiate benign from malignant pulmonary nodules, staging of the cancer by defining involvement of the mediastinum and distant sites, detection of recurrent or residual disease after therapy, and finally to define the prognosis.
FDG is also taken up in tissues that are inflamed and hence infection and inflammatory disorders will show higher activity and are the source of false positives.
The size of the nodule is important since in general only nodules larger than about 7mm can be detected. Standard uptake values (SUV) are a measure of the concentration of a radiotracer. The higher the SUV the greater the accumulation and therefore the higher the metabolic activity. An SUV of 2.5 or greater is more likely to be cancer, and an SUV of less than 2.5 is more likely to be benign disease. Bronchioloalveolar carcinoma however has lower metabolic activity and may even have no uptake of FDG. Well differentiated adenocarcinoma and carcinoid tumors may also have a low SUV.
42244c01
Ashley Davidoff MD
TheCommonVein.net
CT and Lymph Nodes
CT is reported to have a sensitivity of 44 to 79% for detecting mediastinal adenopathy; however, its specificity is low (65%), with “enlarged” nodes sometimes proving to be tumor free.(McCloud). In the past lymph nodes that measured <10mm in the short axis were considered normal. PET scan has disproved this practice since nodes smaller than 10mm in the short axis have been shown to contain metastases. However when the nodes are larger than 10mm in the short axis then the suspicion for metastatic involvement is raised. In the end, PET scanning and then intraoperative biopsy are used to determine staging of the cancer. The presence of lymph adenopathy is an extremely important aspect of the disease since TNM staging is second most important diagnostic consideration after the characterizing the disease into either of the small cell type and or of the non- small type.

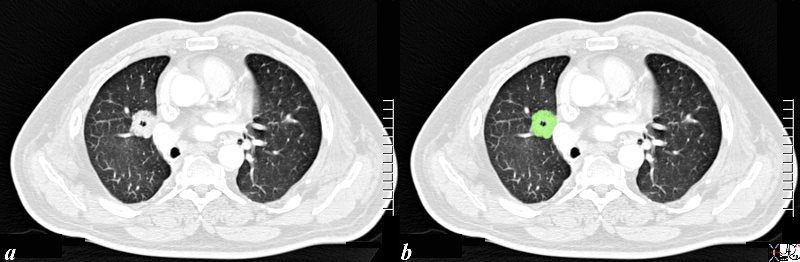
A small nodule (red arrow a,b,c)was identified on the CT in this 60 year old female who is a smoker . The SUV at 1.3 was low (usually >2.5 in malignancy. At pathology it was found to be a necrotizing pneumonia. Most necrotizing granulomas are related to infection. Wegener’s granulomatosis Churg-Strauss syndrome, vasculitis, and sarcoidosis are more often associated with non necrotizing nodules
Ashley Davidoff MD
TheCommonVein.net
72372c03
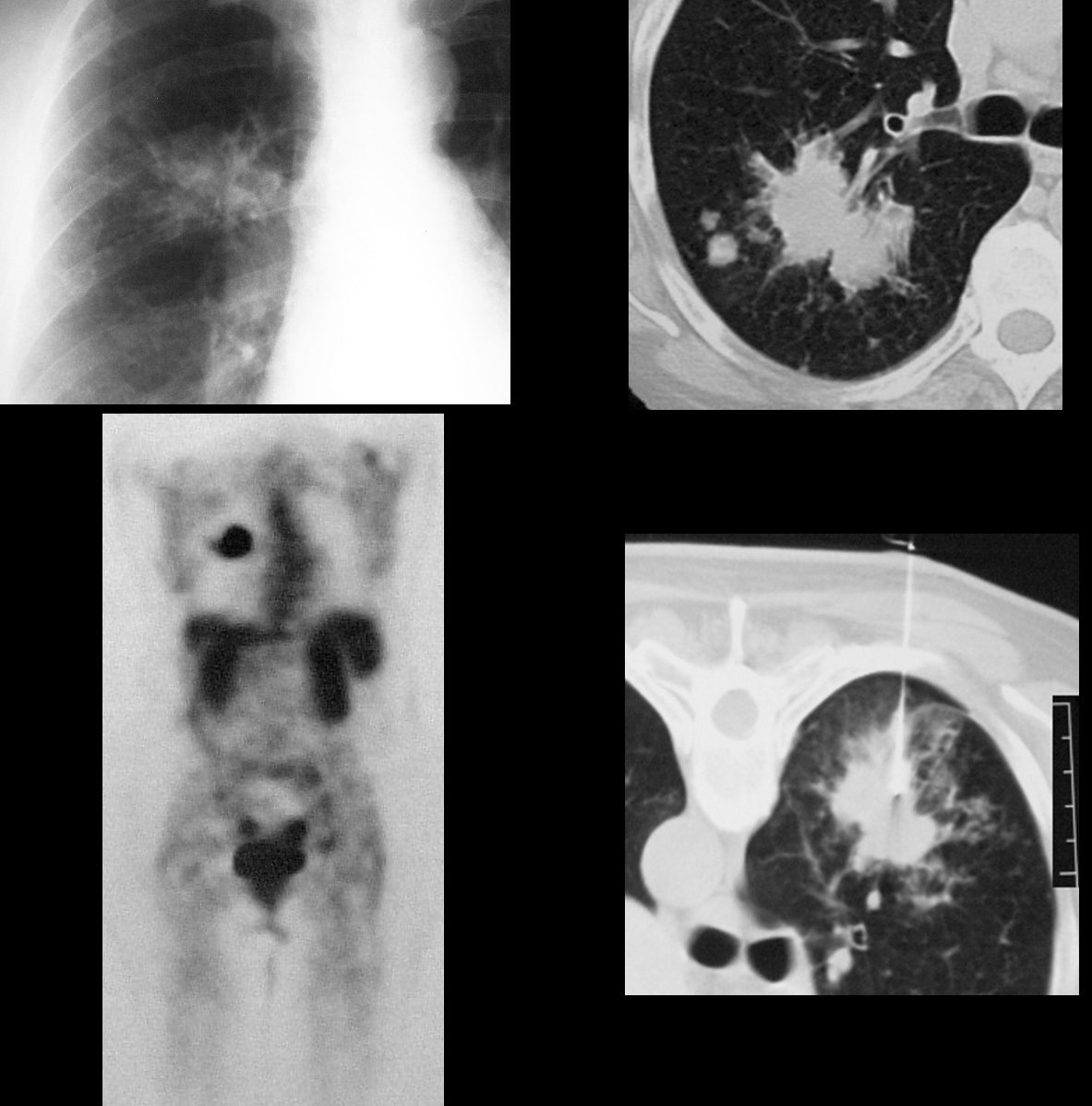
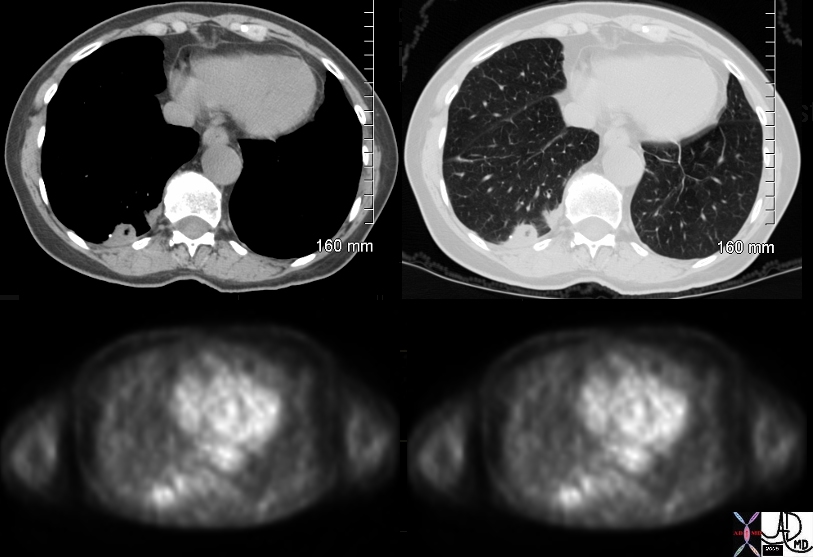
The plain film and CT features of this mass in a 66 year female smoker are concerning for the following reasons; size greater than 3cms, shape with spiculated borders and satellite nodules seen in b. The PET scan was positive and biopsy confirmed the diagnosis. Ashley Davidoff
TheCommonVein.net
28979c
|
False Positive PET Scan |
|
This 60 year old female with granulomatous lung disease presents with chest pain. Rib films were negative. CT scan (a and b) showed a cavitating nodule next to a granuloma. A lung scan was low probability for pulmonary embolism. The PET scan showed increased activity in both nodules with an SUV of 2.1. Pathology showed a subacute and or recent infarction from pulmonary embolism. Courtesy Ashley Davidoff MD 75966c01 |
CT screening
Low dose CT screening is more sensitive than CXR to small nodules, particularly for peripheral lesions. However, false positive rates are high (25% have abnormal tests, only 10% of which are cancers).
PET scans use positron-emitting substances are highly sensitive and specific (greater than 95%) and is the most significant advance in lung cancer diagnosis and staging in recent years. When the mean standardized uptake value (SUV) was equal to or greater than 2.5 the sensitivity, specificity and accuracy were 97%, 82% and 92% respectively.( Duhaylongsod) If the lesion is >10mm sensitivity is up to 95% (Bastarrika). The sensitivity in all lung nodules was only 69%. In patients who have small indeterminate lung nodules (7mm – 2cms), a PET scan is sometimes very helpful particularly if it is negative though issues of false negativity, particulalrly in BAC have to be considered. Although PET has a sensitivity of over 98% with lung cancer it misses 2/3 of patients with BAC (Bunyaviroch).
MRI
MRI appears to be more accurate than CT for demonstrating contiguous invasion of the mediastinum by lung cancers, but this selected advantage is not of sufficient value to use MRI routinely for lung cancer patients.
Ultrasound (US) scans is used mostly as a guide to aspirate pleural fluid.
Links and References
Bone scans have the highest sensitivity to identify metastatic bone disease.