66 y.o. year old male with active smoker (1.5PPD for 30+ years), COPD, Type II Diabetes, and nodular PLCH CD1apositive Langerhans cells on transbronchial biopsy.
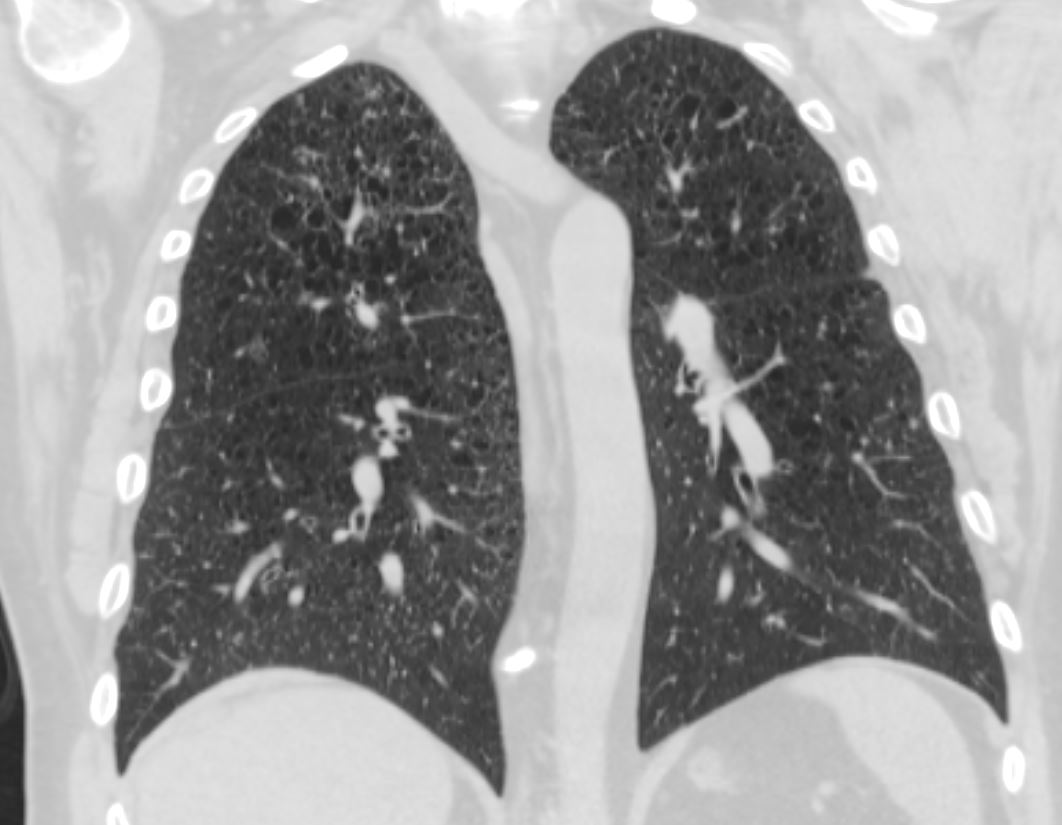
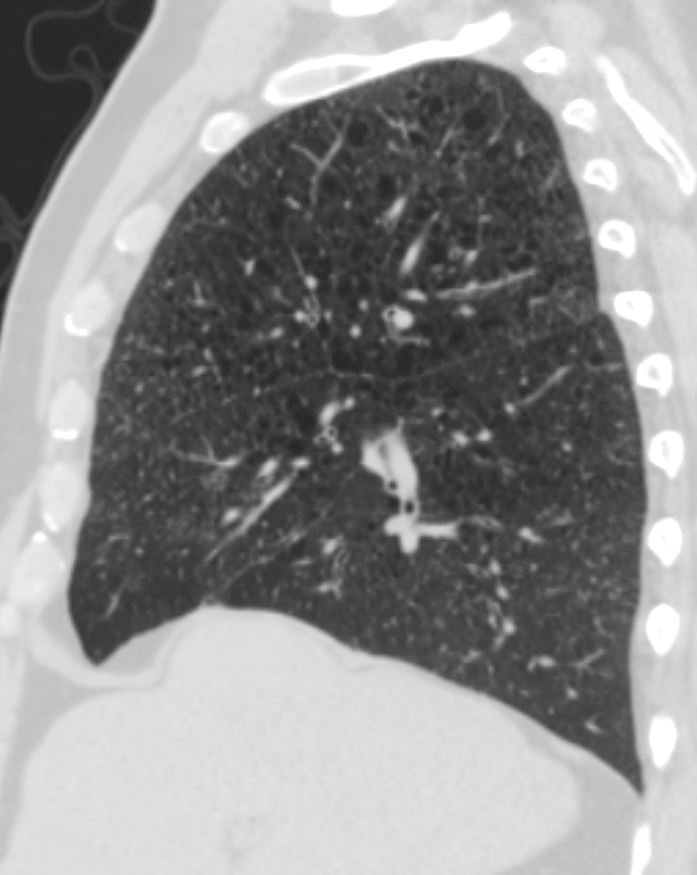
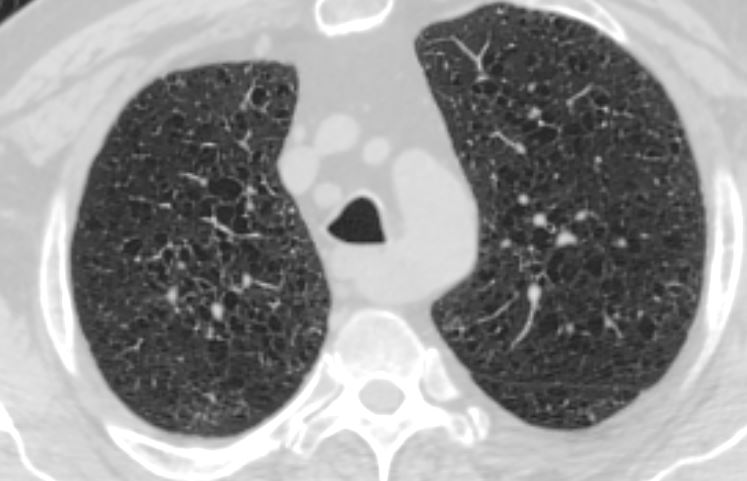
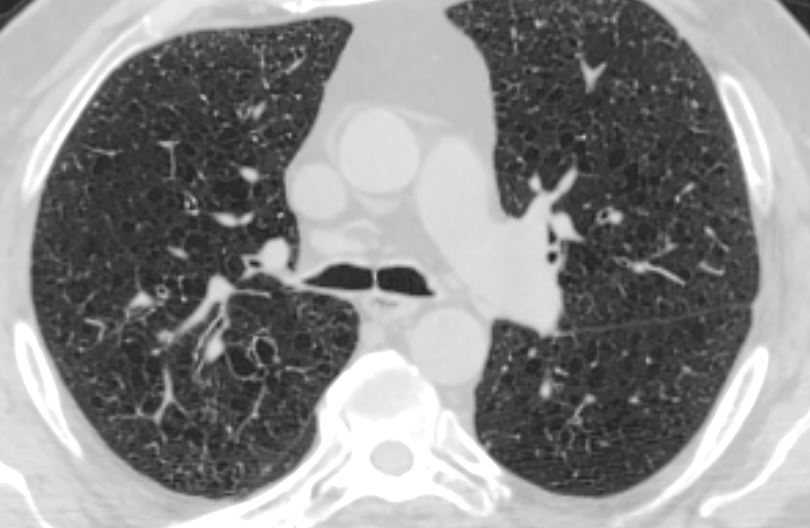
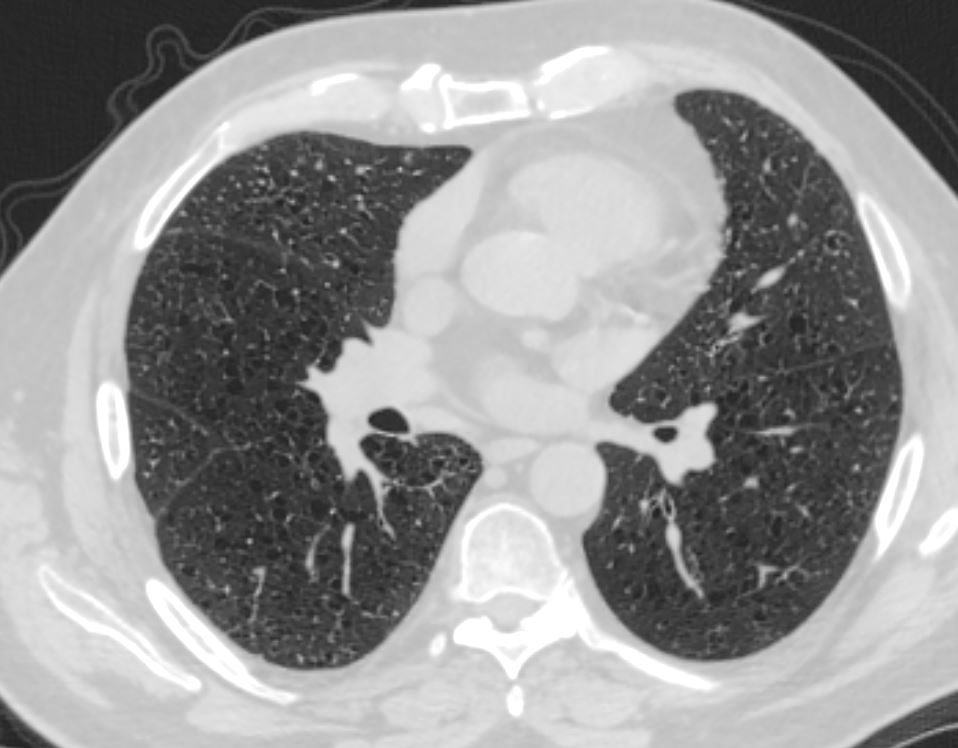
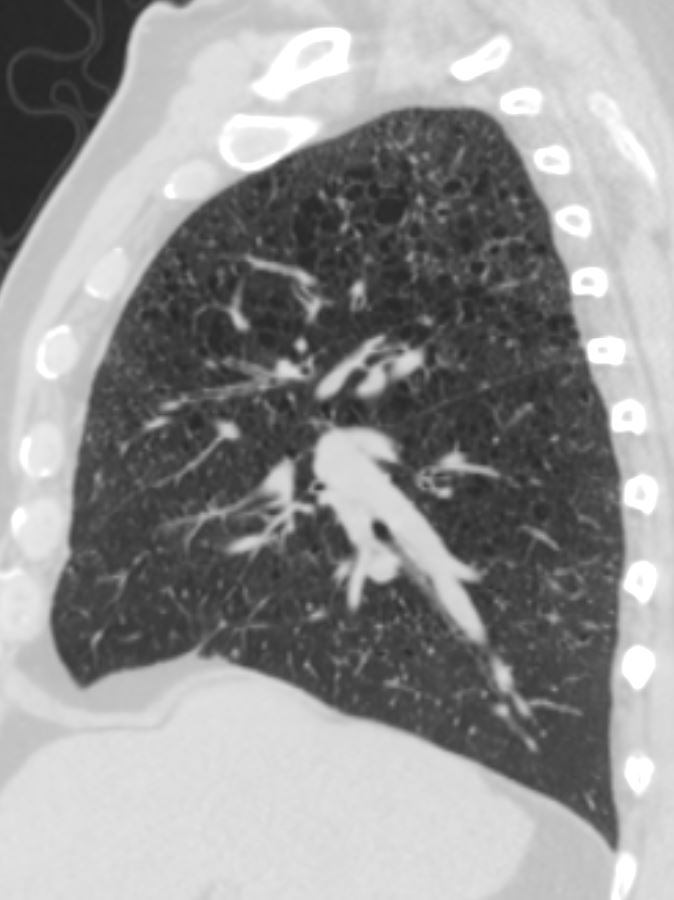
1. There are multiple cysts of various sizes diffusely scattered
bilaterally predominantly in the upper lobes, similar when compared to outside CT images and consistent with known diagnosis of pulmonary Langerhans’ cell histiocytosis.
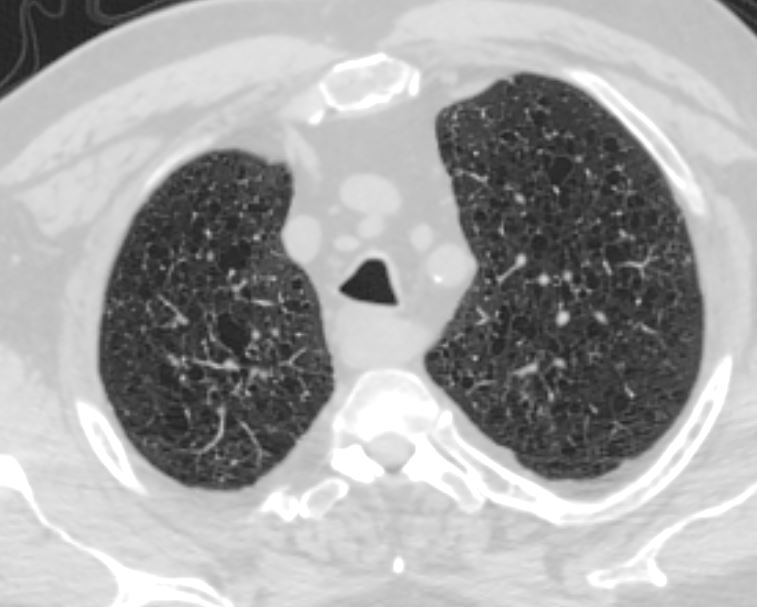
2. There are innumerable centrilobular and intralobular nodules most notable in the lower lobes, in addition to multifocal peripheral
tree-in-bud nodules suggestive of bronchiolitis due to
inflammation/infection. The micronodules are better appreciated on the study and this represents progression versus technique differences is not certain.
Sparing of the posterior recesses is consistent with the diagnosis
pulmonary Langerhans’s cell histiocytosis
3. No evidence of air trapping
4. Multiple solid nodules measuring up to 4 mm
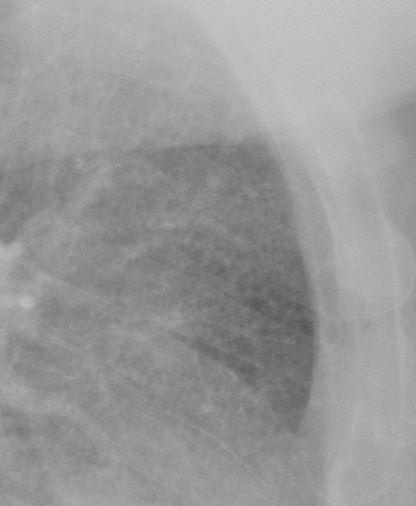
CXR PA – Suggestion of Interstitial Disease and Cystic Changes
As noted on CT the recesses are spared
CXR Lateral – Suggestion of Interstitial Disease and Cystic Changes anteriorly
As noted on CT the recesses are spared
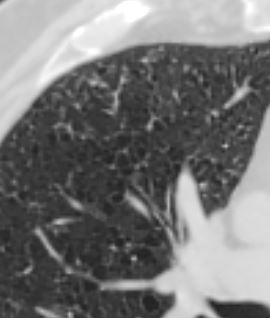
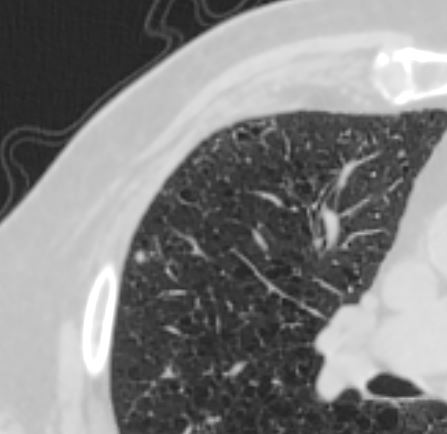
Multiple variably sized, mostly thin walled cysts and micronodules dominant in the upper lobes
Some scattered thicker walled cysts
Medium sized airway thickening extending into the small airways
Centrilobular Nodules tree in bud and intralobular nodules
Other 2-4 mm nodules
Lung bases dominated by microndules – Paucity of Cystic Changes
Sparing of the posterior recesses
Expiration – Shows no air trapping
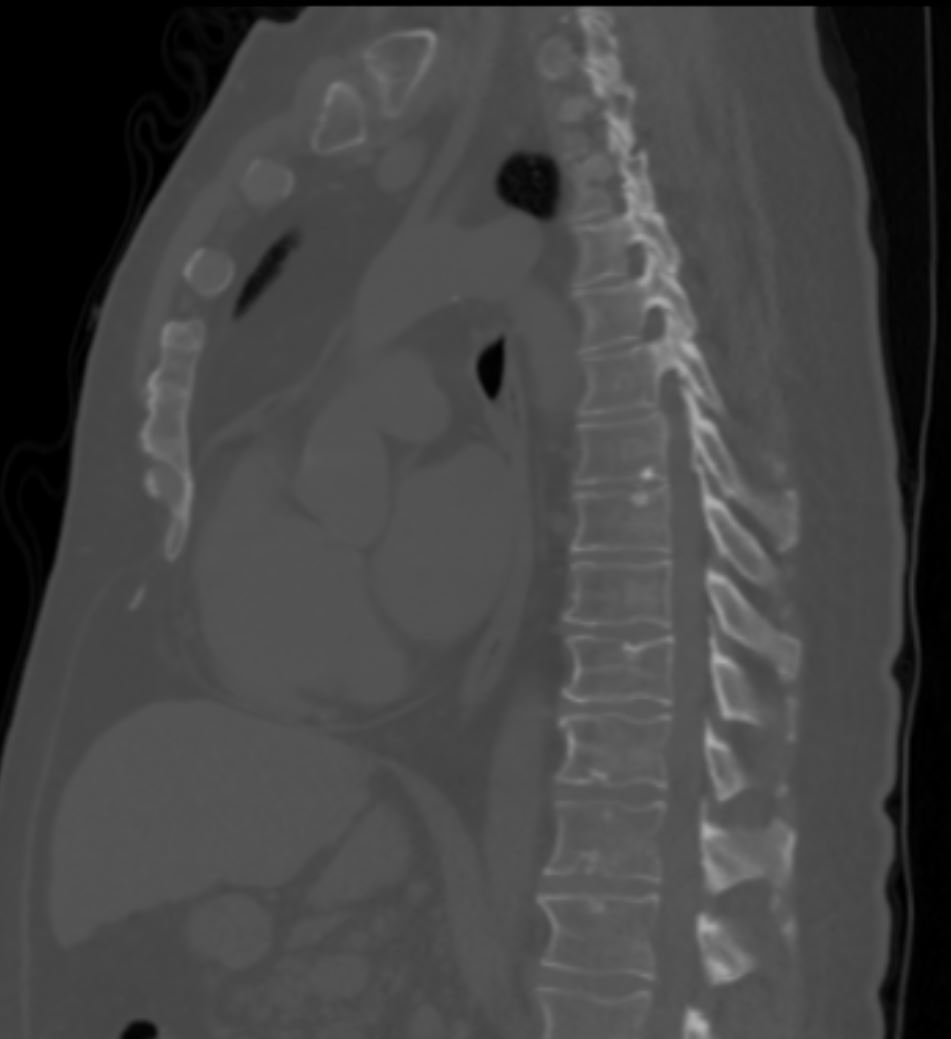
Sclerotic Bone Disease in the mid thorac spine – possibly related to Pulmonary Langerhans Cell Histiocytosis but may just be a benign bone island and or end plate sclerosis
Ashley Davidoff MD TheCommonVein.net