50 m year old female with combined variable immunodeficiency syndrome
- 49 y.o. female
- hx of
- sinusitis, pneumonia, and bronchitis. bronchiectasis in setting of CVID.She was diagnosed with low IgG around 19 years ago and started on IgG replacement in 4 years later, the transitioned
- Diagnosed with CVID due to low IgA and, later, low IgM.
- hx of
3 years ago
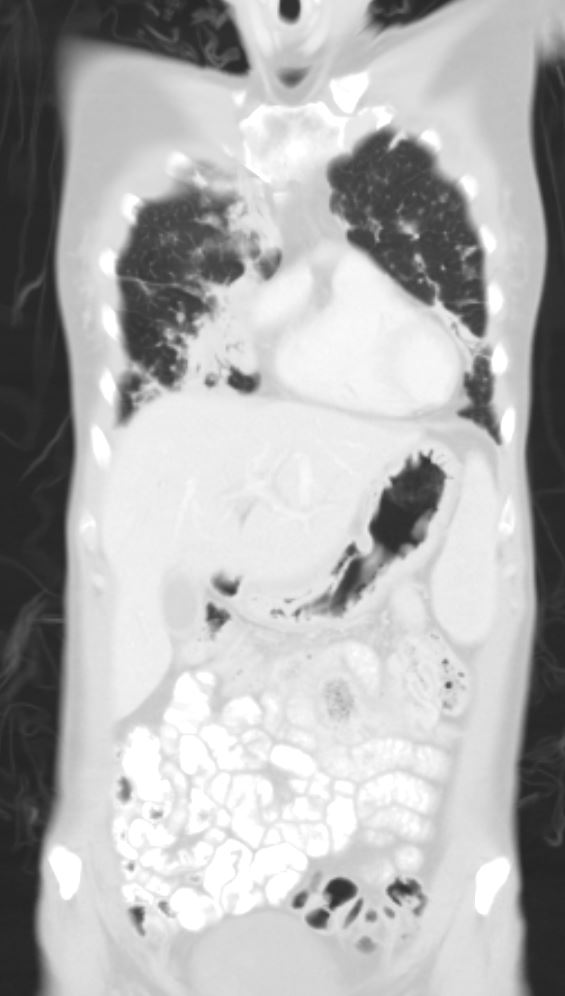
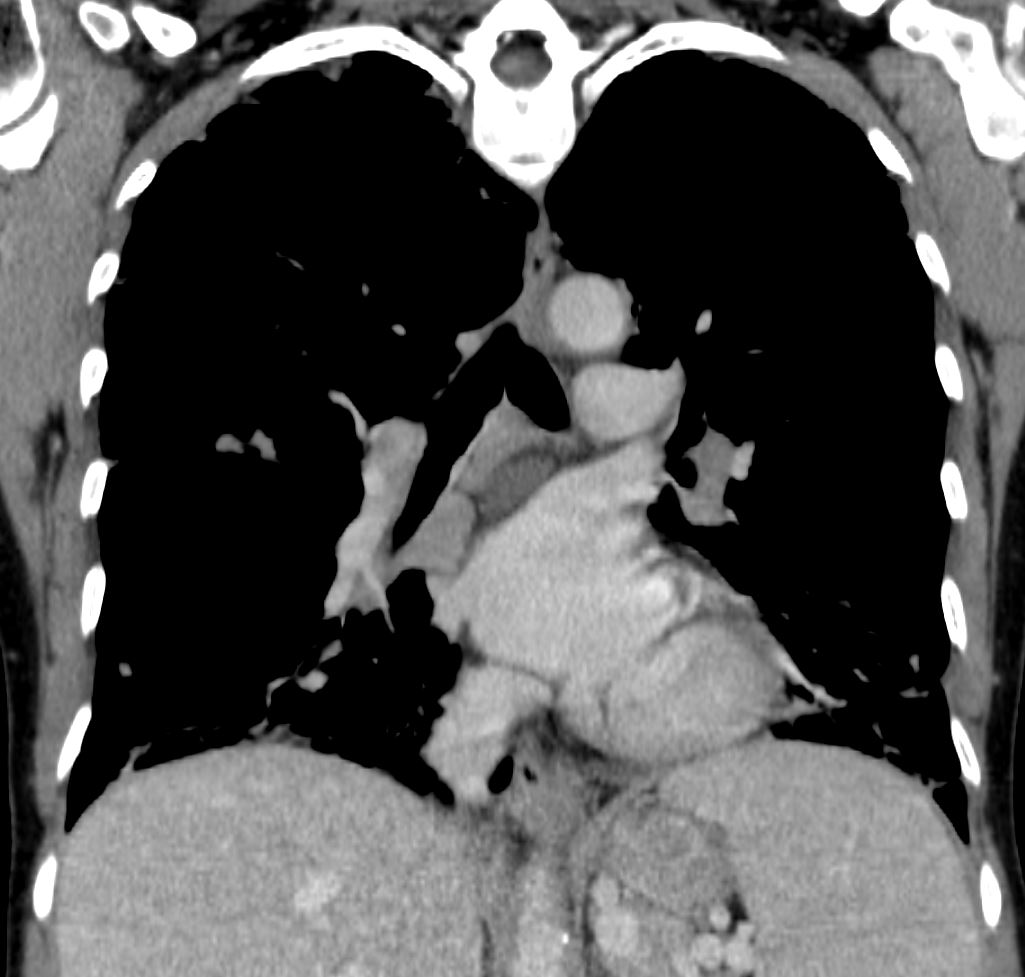
Pulmonary Nodules and lymph – adenopathy splenomegaly
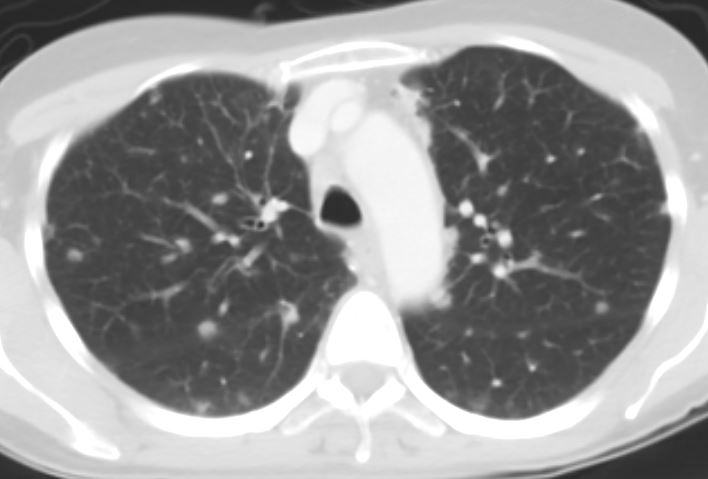
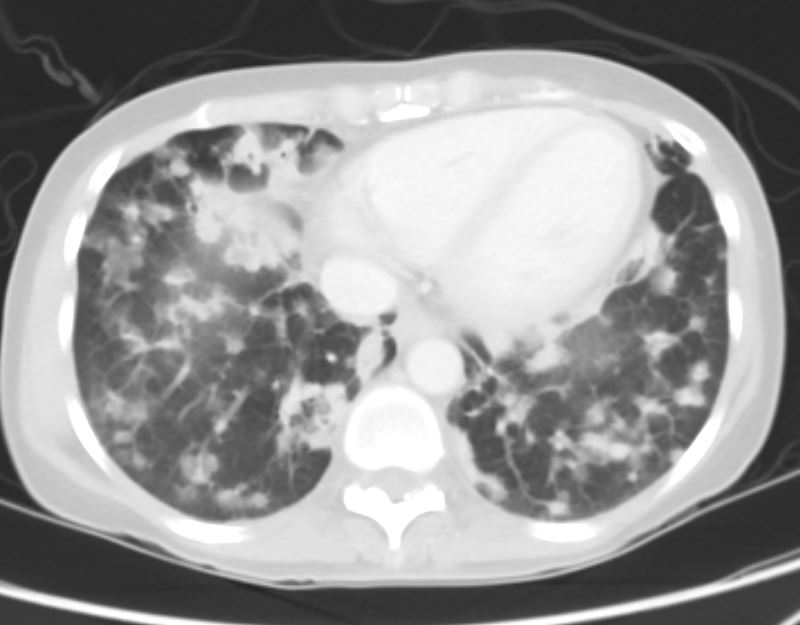
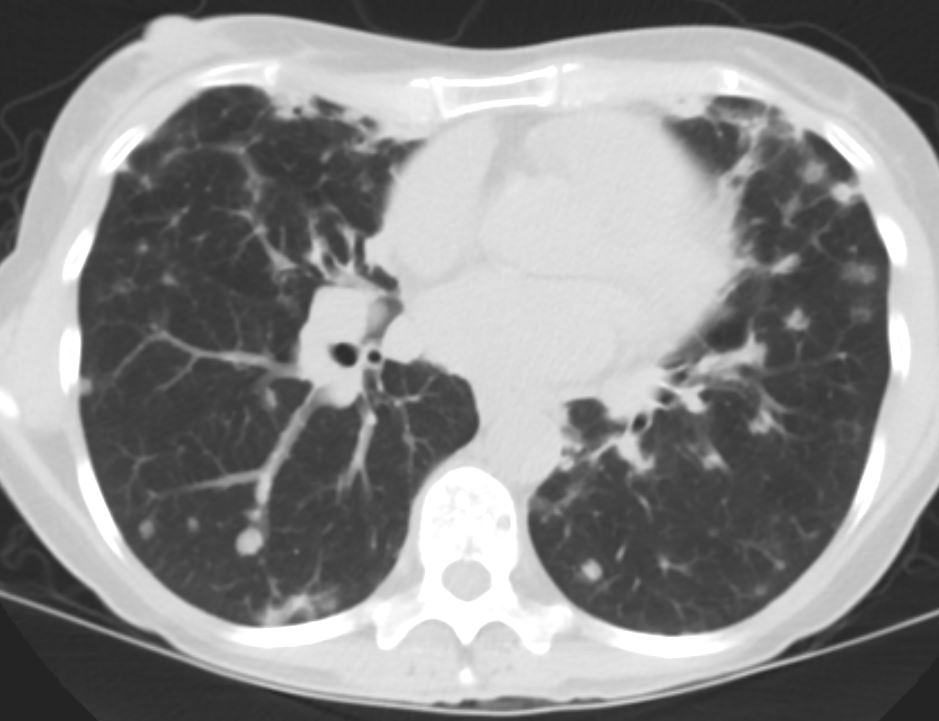
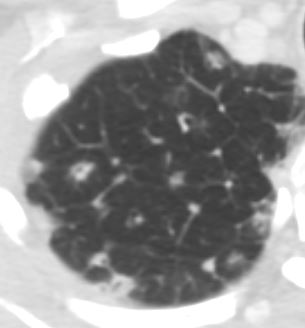
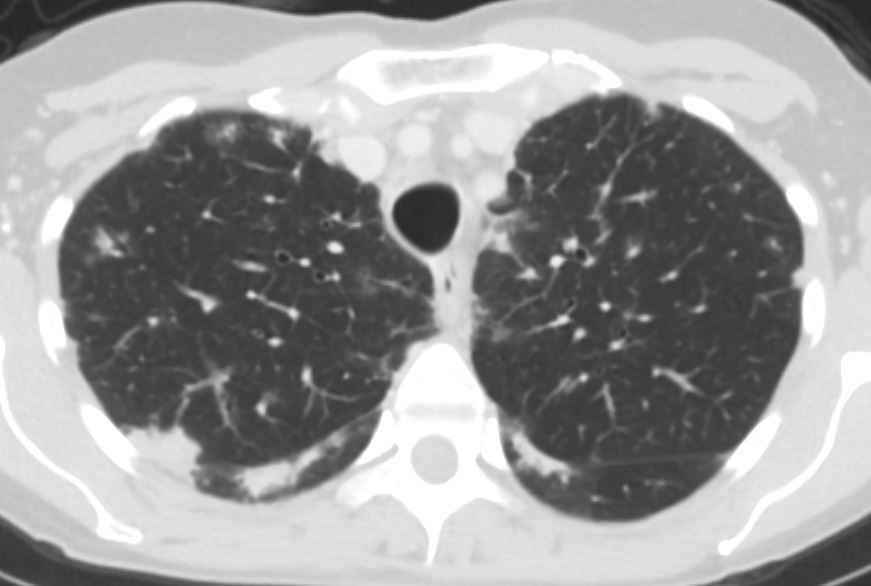
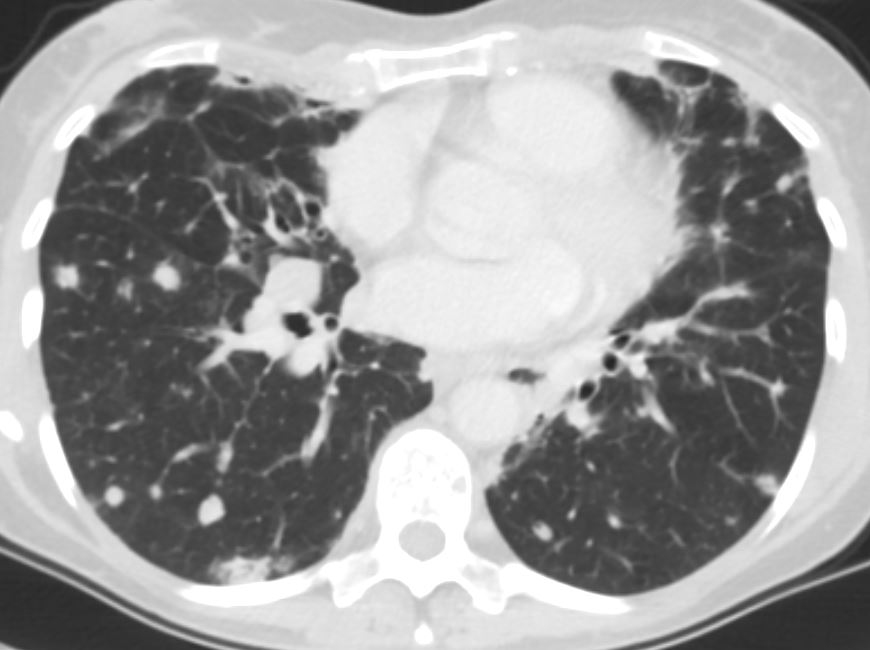
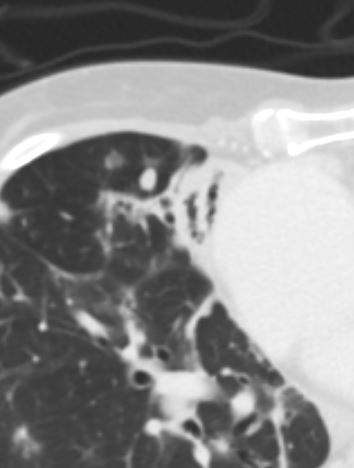
- CT chest from 3 years ago
- Interval increase in the size and number of numerous pulmonary nodules with
- basal predominance compared to the prior
- consistent with granulomatous lymphocytic interstitial lung disease
- ? underlying/superimposed infection
- stable bronchiectasis and consolidation in the medial right middle lobe and lingula.
- Stable bilateral hilar lymphadenopathy.
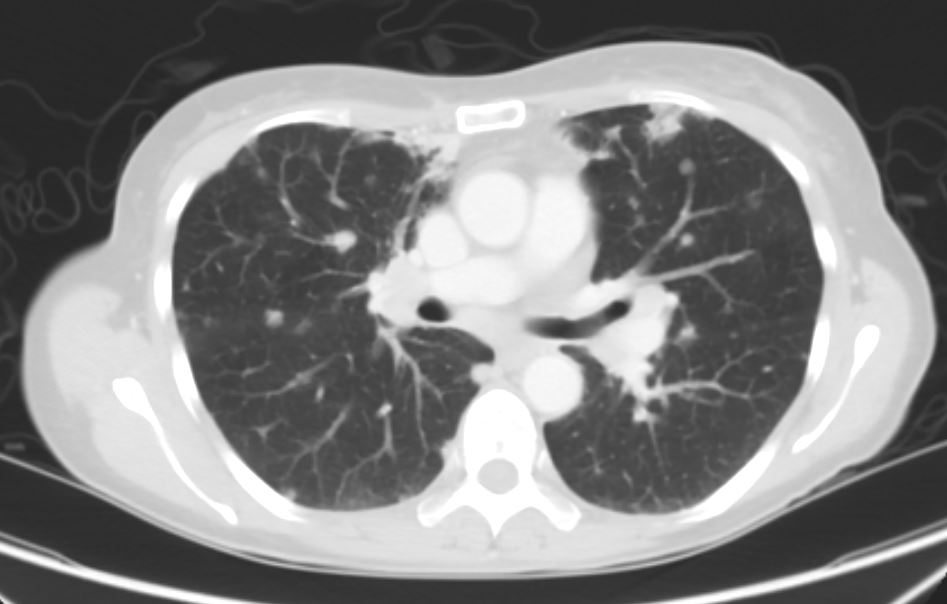
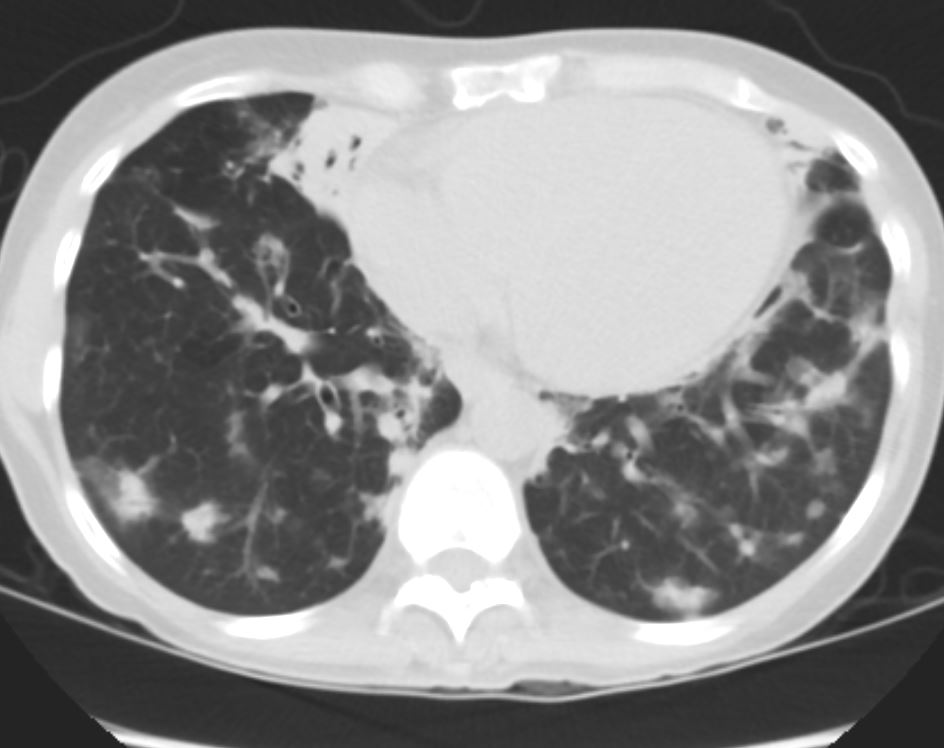
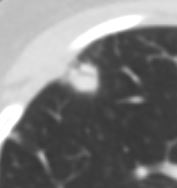
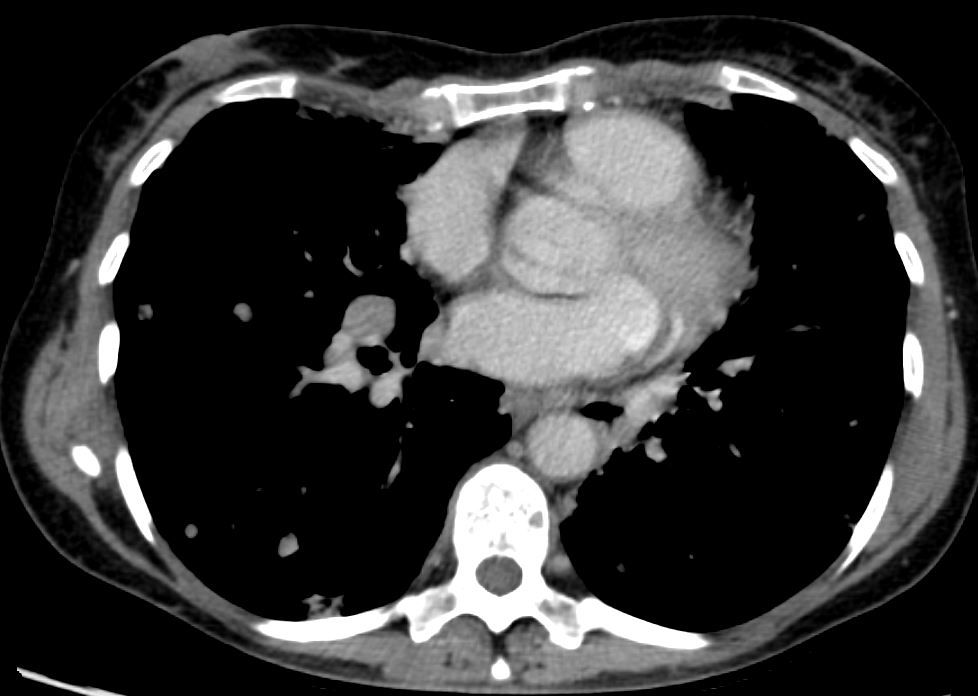
1 year ago
Unchanged Symptoms
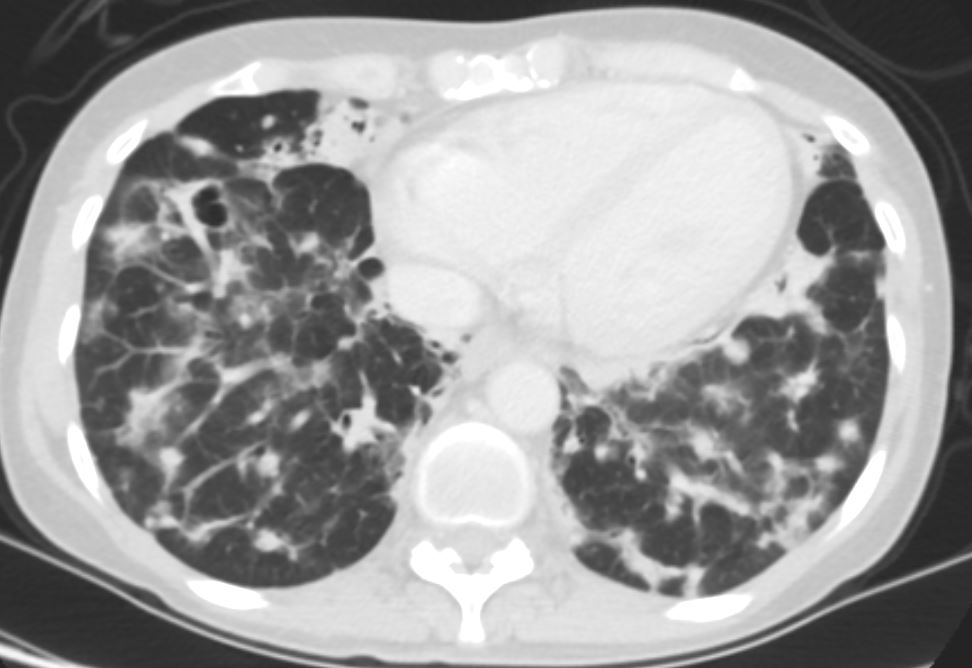
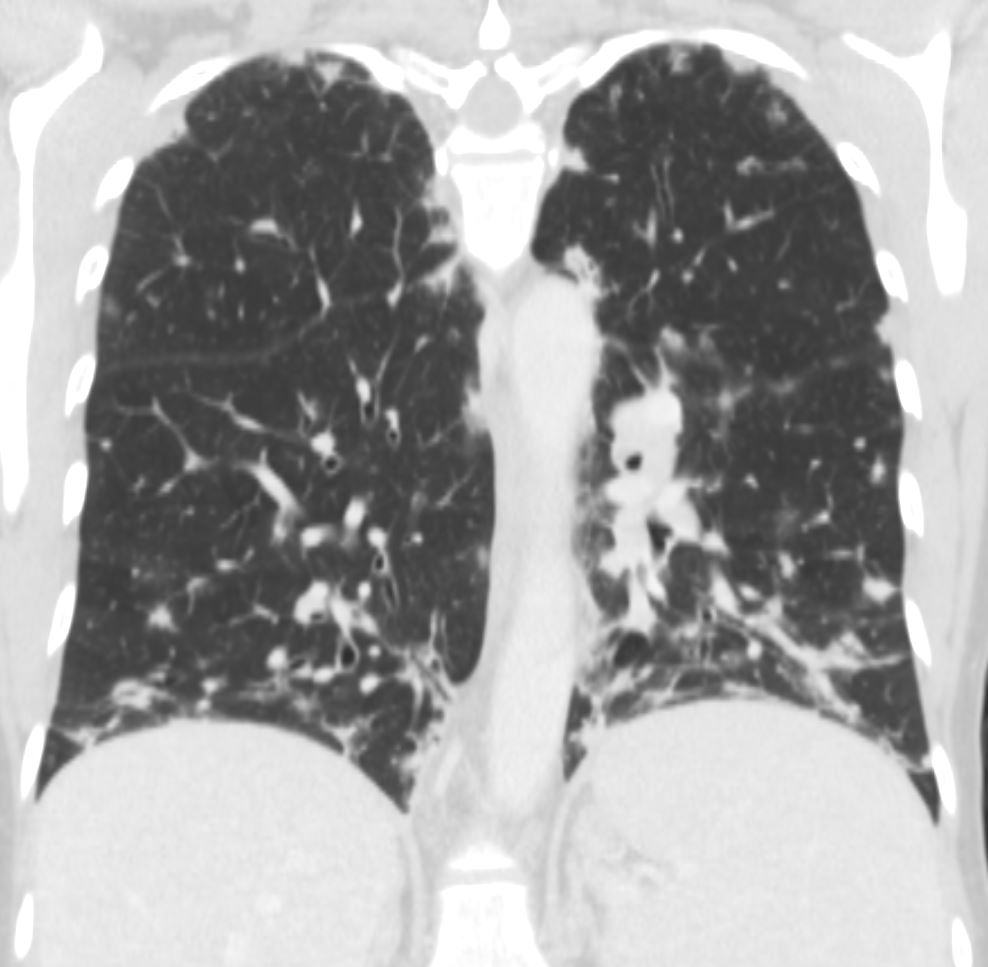
- Interval increase in size, confluence, and number of irregular widespread pulmonary nodules.
- suggestive of progressive granulomatous lymphocytic interstitial lung disease.
- Stable right middle lobe and lingular peribronchial consolidations with bronchiectasis.
- Stable mediastinal and hilar adenopathy.
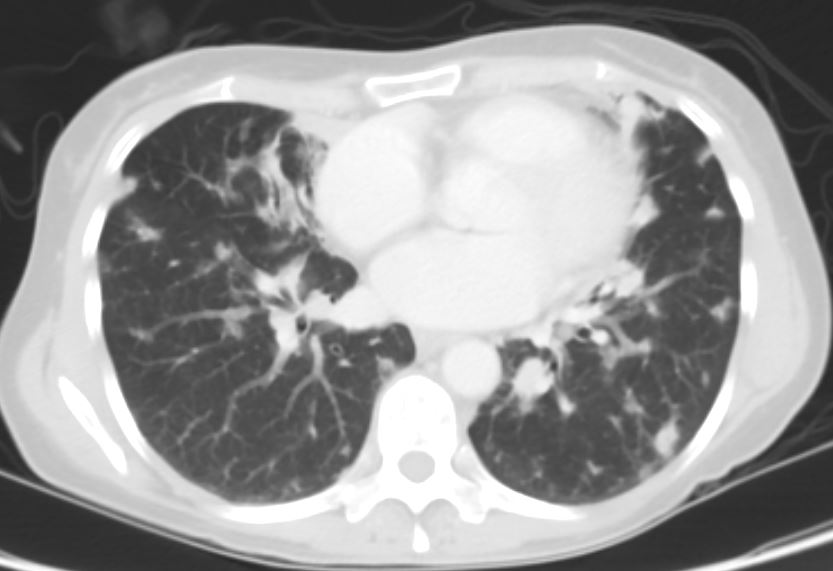
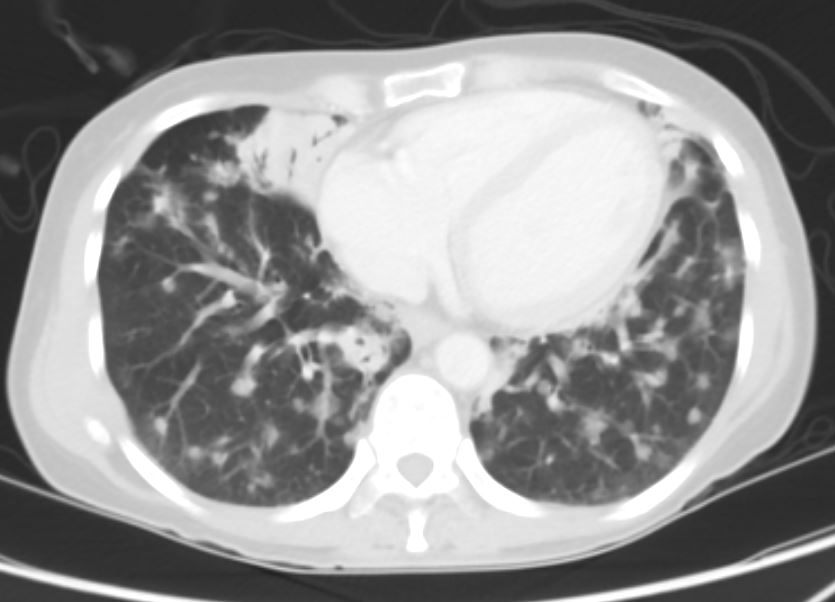
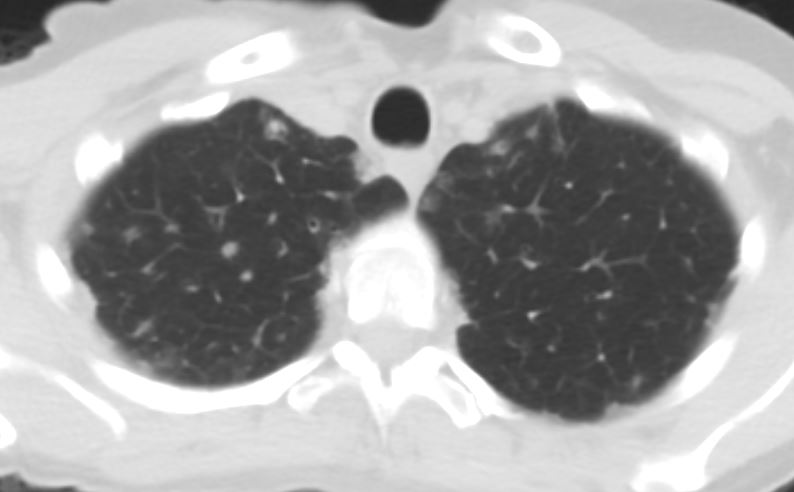
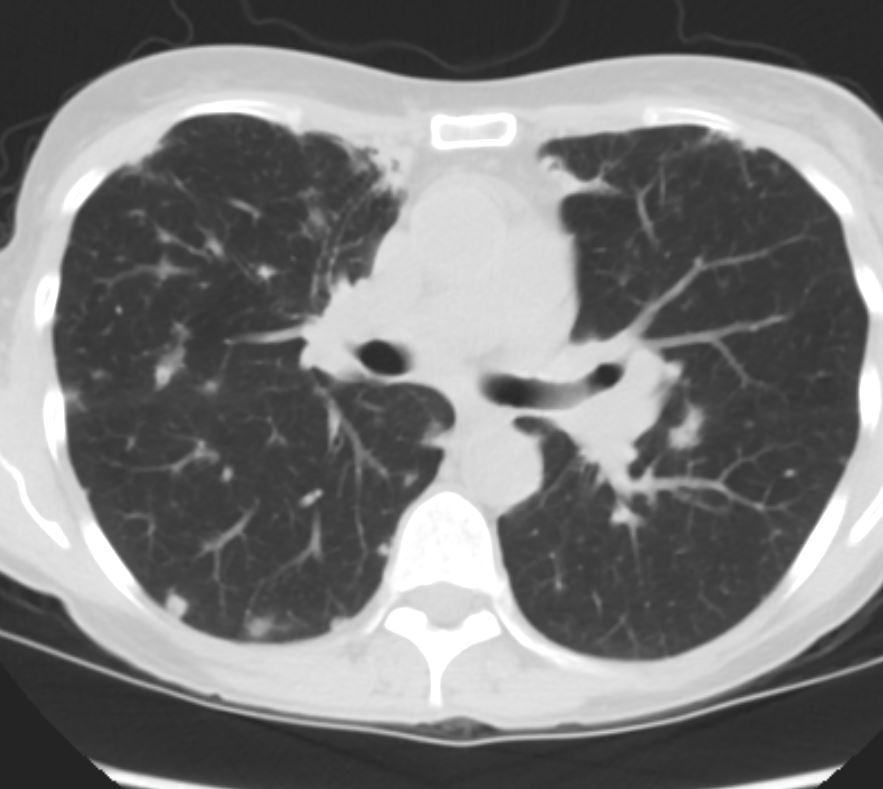
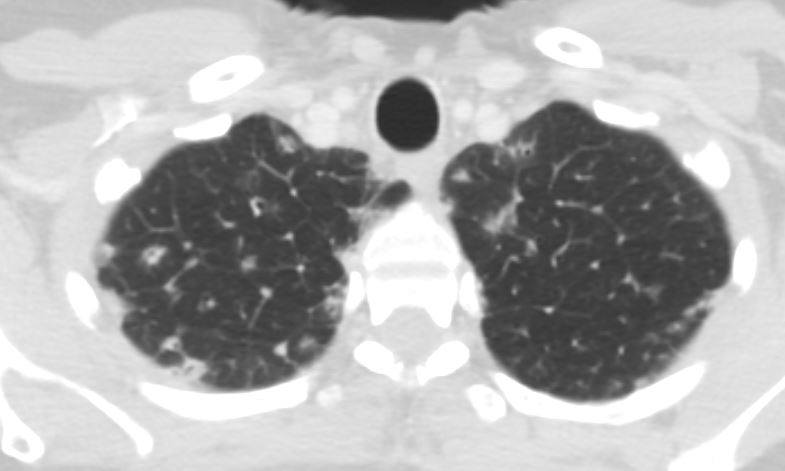
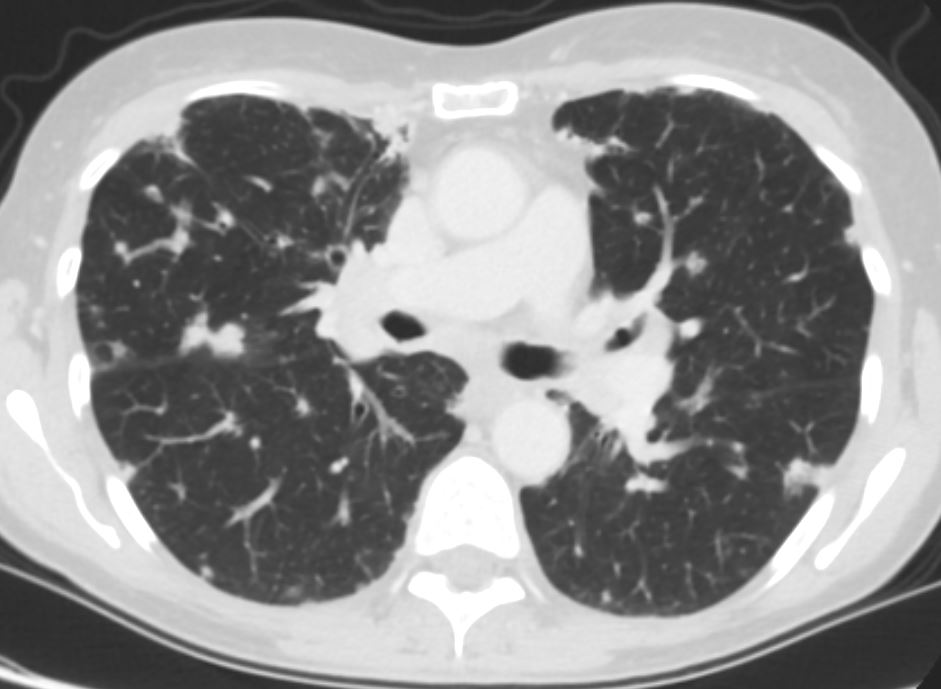
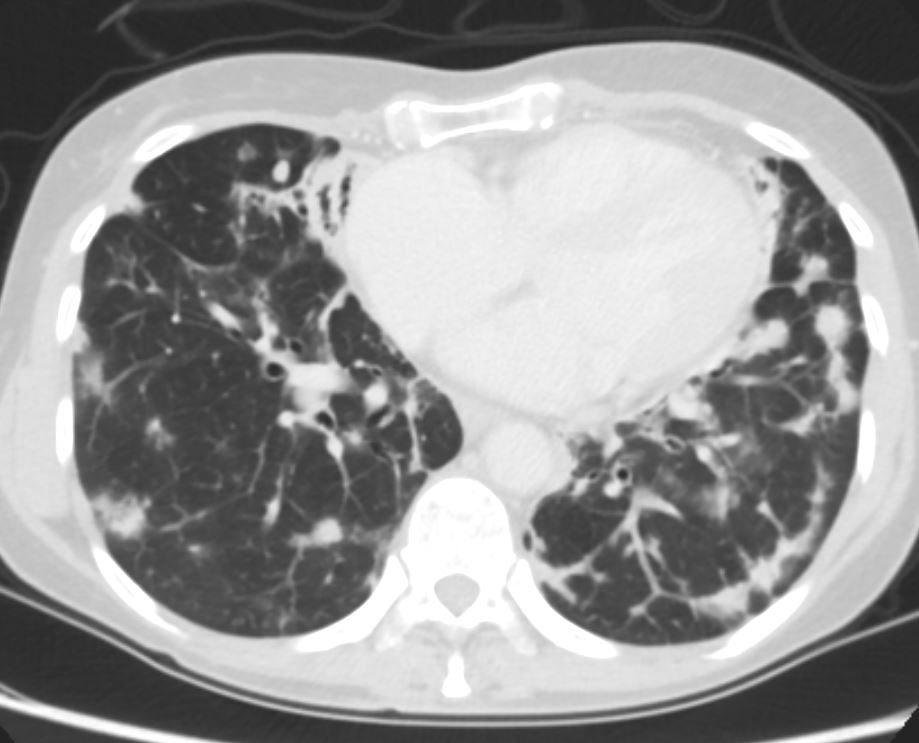
Current
- lack of fever or acute deterioration,
- growth of the only normal upper respiratory flora on the recent sputum culture
- Sputum culture negative
- Imaging shows progressive
- granulomatous interstitial lung disease (GL ILD) and
- lymphocytic interstitial lung disease
- associated with CVI D
- bronchiectasis
- associated with CVI D