Blood Supply to the Lungs
- Blood vessels in the lower lung fields are larger than those in the upper lung fields.
- The lower lung fields require a greater blood supply due to their greater role in gas exchange.
- Gravity plays a role in the distribution of blood flow, causing blood to pool in the lower parts of the body, including the lower lobes of the lungs.
- The larger blood vessels in the lower lung fields are better equipped to handle the increased blood flow caused by gravity and to perfuse the lower lobes of the lungs.
- Lung tissue in the lower lobes is denser and has more alveoli per unit of volume, requiring a larger blood supply to adequately oxygenate the larger volume of gas exchange tissue.
Efficiency of Gas Exchange
The lower lobes of the lungs are generally considered to be more efficient than the upper lobes in terms of gas exchange. This is due to a number of factors related to the anatomy and physiology of the lungs.
First, the lower lobes have a larger surface area for gas exchange than the upper lobes. This is because the lower lobes have a higher concentration of alveoli (the tiny air sacs in the lungs where gas exchange occurs) per unit of lung tissue compared to the upper lobes. This increased surface area allows for more efficient transfer of oxygen and carbon dioxide between the lungs and the bloodstream.
Second, the lower lobes have a greater perfusion (blood flow) than the upper lobes. This means that the blood vessels in the lower lobes are larger and more numerous, allowing for more efficient delivery of oxygen to the lung tissue and removal of carbon dioxide.
Finally, the lower lobes are more gravity-dependent than the upper lobes, meaning that they receive a greater volume of air during normal breathing due to their lower position in the chest. This increased ventilation allows for more efficient gas exchange in the lower lobes.
Overall, while all parts of the lungs are important for gas exchange, the lower lobes are generally considered to be more efficient due to their larger surface area, greater perfusion, and increased ventilation.
Oxygen Tension
The oxygen tension (partial pressure of oxygen, or PO2) is generally higher in the upper lobes of the lungs compared to the lower lobes.
This is because the upper lobes receive a greater volume of air during normal breathing, which contains a higher concentration of oxygen compared to the residual air left in the lungs after exhalation. Additionally, the upper lobes have a lower concentration of carbon dioxide compared to the lower lobes due to differences in ventilation and perfusion.
However, it is important to note that the distribution of oxygen tension in the lungs can vary depending on factors such as posture, exercise, and lung disease. In some cases, such as in lung disease, the distribution of oxygen tension may be more uniform across the lung fields or may be lower overall compared to healthy lungs.
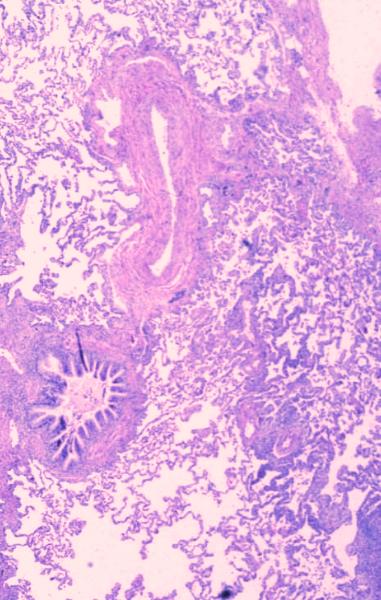
This histological section shows the bronchovascular bundle in their true form. We are still fairly proximal since you can see the much smaller alveoli and alveolar ducts in the background. The mucosa of the bronchiole is thrown into a series of folds while the endothelium of the arteriole smooth and the lumen is collapsed.
Courtesy Armando Fraire MD 32699b
When we speak of an artery, we tend to think of a high pressured system with oxygenated blood. The common characteristic that defines them however is the fact that they carry blood away from the heart and toward an end organ. Hence the pulmonary artery, true to definition, carries blood away from the heart, but it is deoxygenated and is under relatively low pressure.
The pulmonary circulation receives more blood per minute than any other organ in the body since it receives the entire cardiac output from the right ventricle, together with a small component (1-2% of total pulmonary blood flow) from the bronchial arterial flow.
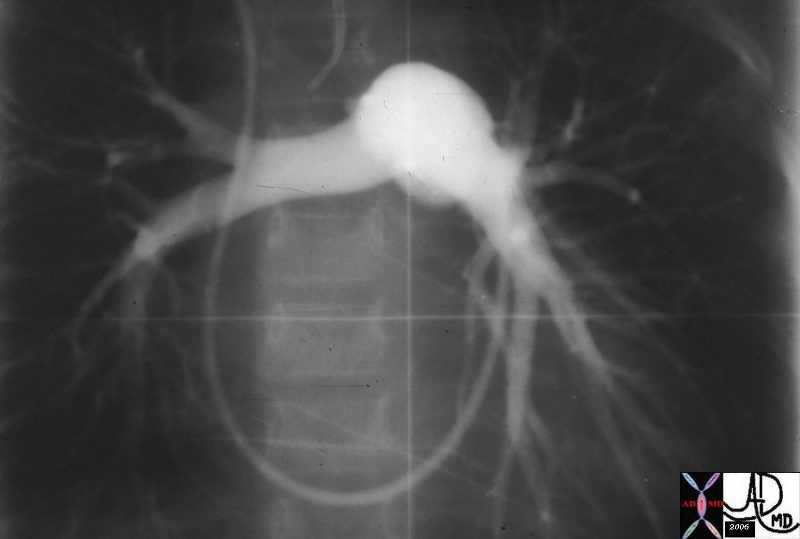
Normal pulmonary angiogram demonstrating the asymmetric positioning and course of the left pulmonary artery which has a downward and vertical course, whereas the RPA assumes a more horizontal course.01560.800 Ashley Davidoff MD TheCommonVein.net
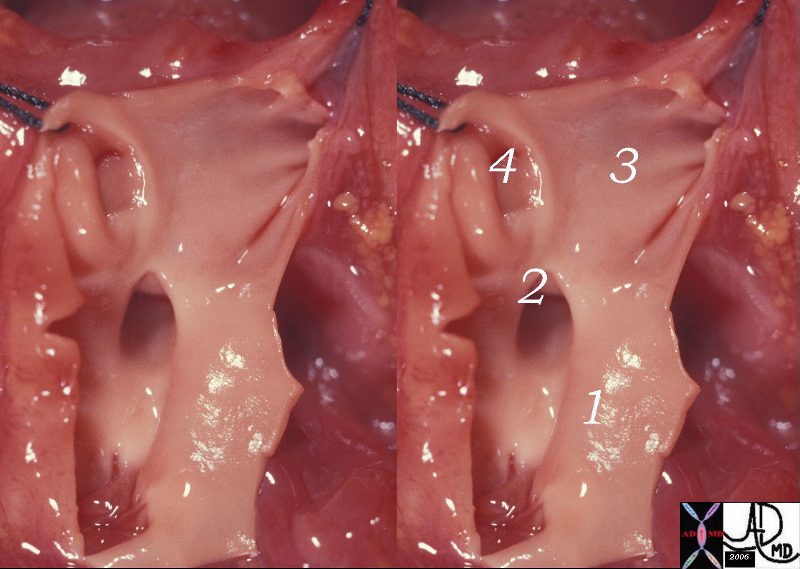
The anatomic specimen is from a neonate with a normal cardiovascular examination and demonstrates a normal pulmonary valve main pulmonary artery (1), RPA (2), LPA (3) and a ductus arteriosus that is still patent (4)32625c01 Ashley Davidoff MD TheCommonVein.net
The right ventricular outflow tract (RVOT) gives rise to the MPA which in turn divides into left and right pulmonary arteries. We have noted the difference in the anatomy of the right and left mainstem bronchi (right short and fat, left long and thin), and the similarity in the branching patterns of the distal bronchi and distal arterial system. While the RPA and LPA are similar in size they bear no resemblance to each other nor to the mainstem bronchi.
On a frontal view CXR we are able to identify and measure the descending right pulmonary artery
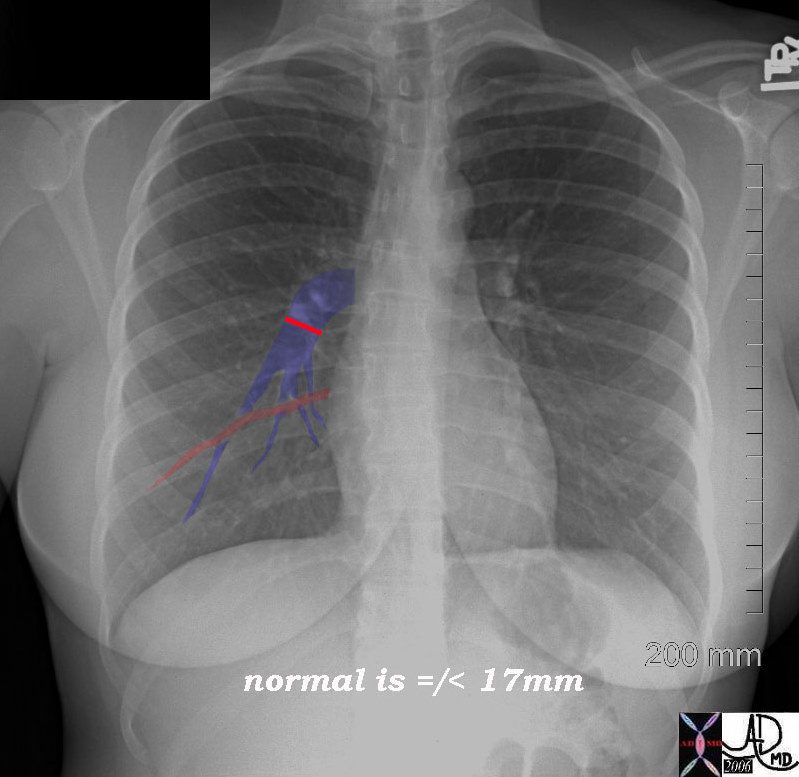
Ashley Davidoff MD TheCommonVein.net 45756d04
The left artery has great athletic ability as evidenced by its ability to high jump over the left main stem bronchus. (the hyparterial bronchus) The right does not make it over the right mainstem, and is satisfied to sneak under the right main stem bronchus (the eparterial bronchus).
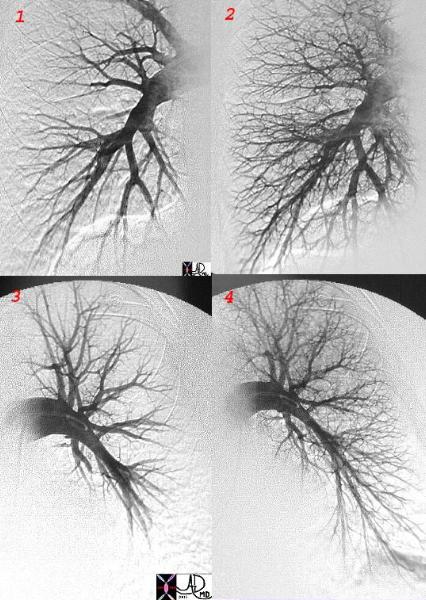
This is a normal pulmonary angiogram in the arterial phase and the arteriolar phase with image 1 and two representing these phases in the right system, and images 3 and 4 the phases within the left arterial system.
Ashley Davidoff MD TheCommonVein.net 27655 c
If you recall the LPA has the ability to high jump over the left mainstem bronchus, while the RPA has to be satisfied with a jump between bronchus intermedius below and the RUL bronchus above.
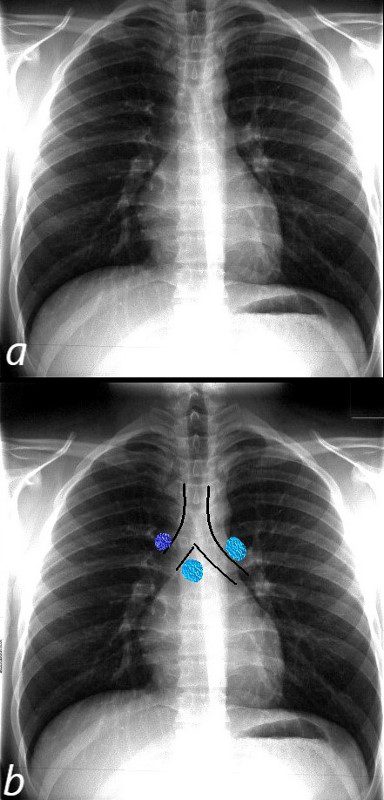
The normal CXR shows the superior position and relationship of the LPA to the left mainstem bronchus. The bronchus is hyparterial ie below the artery.
The RPA (light blue and right in b) runs below the right mainstem bronchus ie the bronchus is eparterial . The azygos vein lies superior to the right mainstem bronchus at the take off of the right mainstem from the trachea.
Ashley Davidoff MD TheCommonVein.net
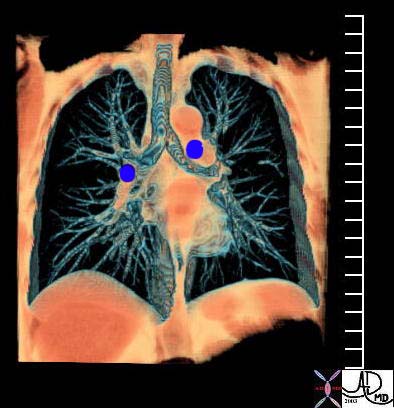
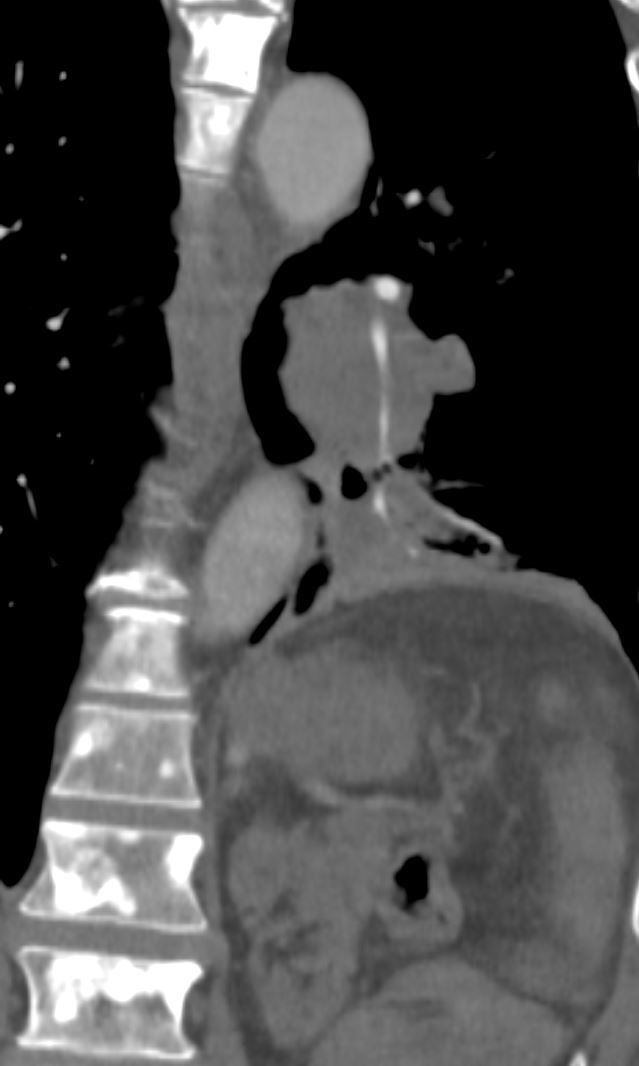
This coronal reformat shows the position of the main branch pulmonary arteries relative to the position of their respective bronchi. While the RPA runs under the right mainstem bronchus, the LPA runs above the left mainstem.
Courtesy Ashley Davidoff MD TheCommonVein.net 32620b01
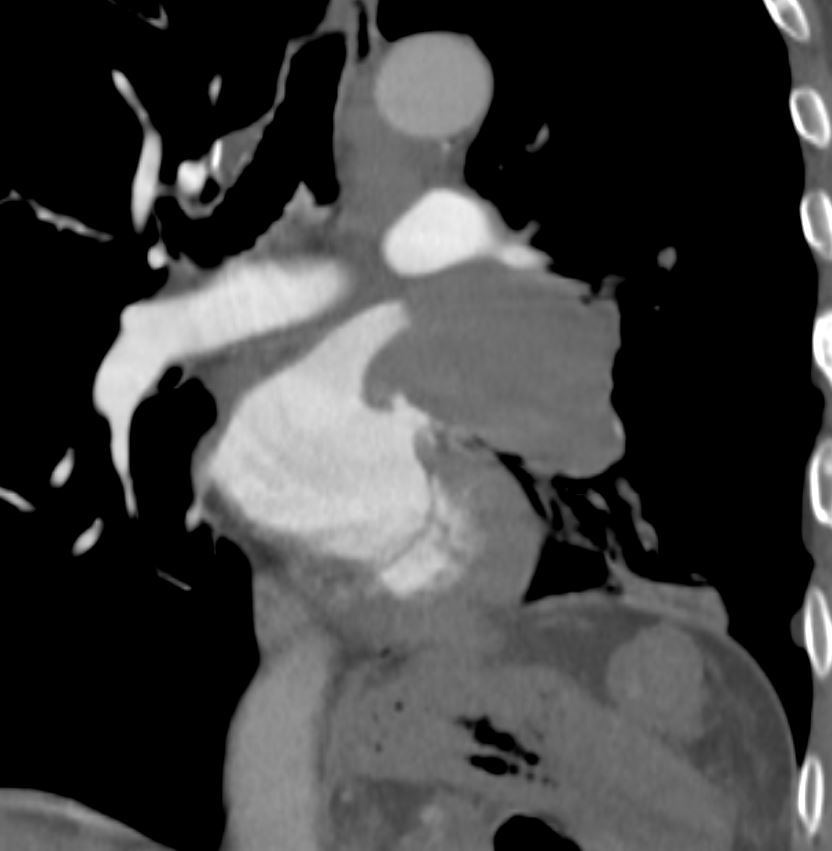
The direction that the two vessels are oriented is also completely different. The LPA courses directly posteriorly while the RPA courses directly laterally.
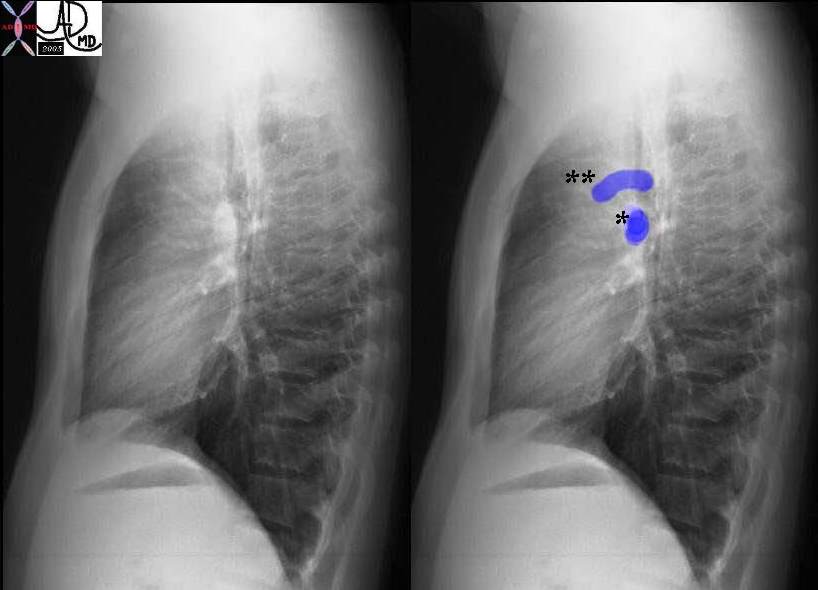
The lateral examination serves to demonstrate the ovoid appearance of the right pulmonary artery (*) as it courses above the LA to the right midaxillary line, together with the more cranially placed arching shape of the LPA (**) which courses posteriorly. Courtesy Ashley Davidoff MD TheCommonVein.net 30398c04
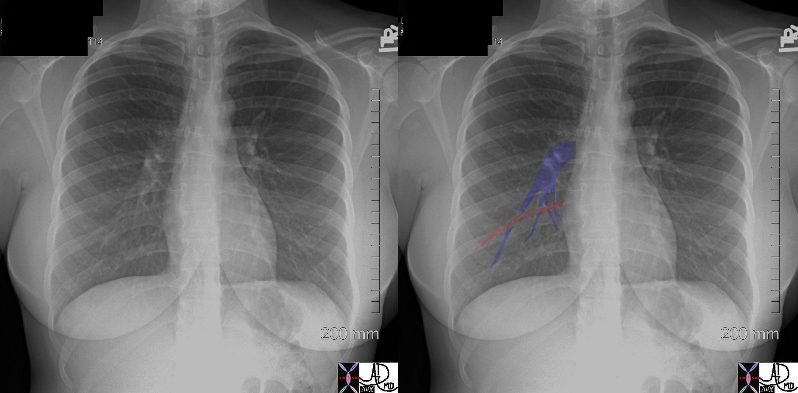
The pulmonary veins of the RLL can be seen running horizontally toward the LA while the PA’s to the RLL run a more vertical course.
Courtesy Ashley Davidoff MD TheCommonVein.net 45756c01b
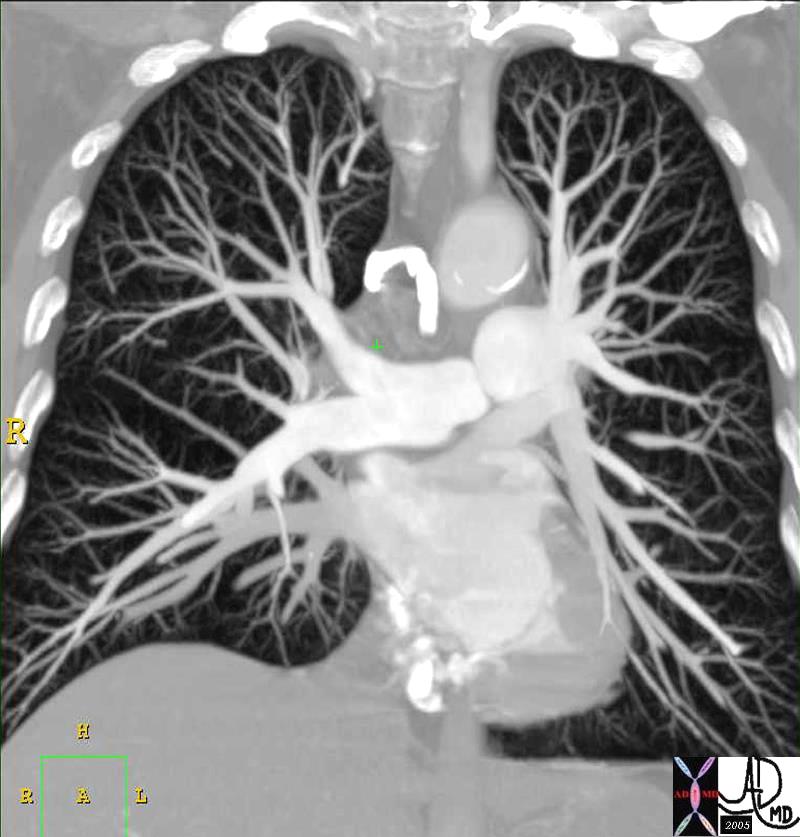
In this coronally oriented CTA the RPA can be seen traveling horizontally above the LA and the LPA origin hides behind the MPA as it courses posteriorly. Courtesy Ashley Davidoff MD TheCommonVein.net 32807
In this coronally oriented CTA the RPA can be seen traveling horizontally above the LA and the LPA origin hides behind the MPA as it courses posteriorly. Courtesy Ashley Davidoff MD TheCommonVein.net 32807b03.8s
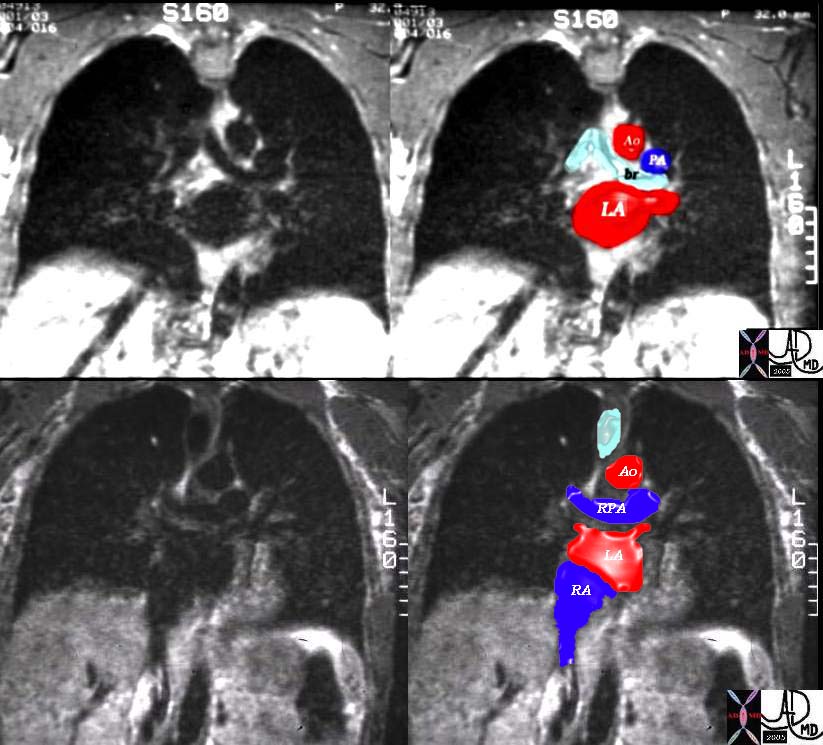
The right pulmonary artery (RPA) takes almost a 140-degree turn from the main pulmonary artery. It rests on the top of the left atrium (LA) and has a straight shot in the direction of the midaxillary line. Thus on a lateral examination of the chest the LPA has the shape of an umbrella handle and the RPA is seen as an ovoid or rounded structure as we look down its barrel. The pulmonary veins are all inferior to the pulmonary arteries at the hilum.
Distal to the main pulmonary arteries, the branches follow the branching of the irregular dichotomous branching of the airways, and their morphology is similar till they enter the pulmonary lobule at the level of the respiratory bronchiole. At the capillary level, all the blood supplied by the pulmonary artery drains into the alveolar capillaries where they become oxygenated and then drain into the pulmonary venules within the interlobular septa, and finally back to the left atrium.
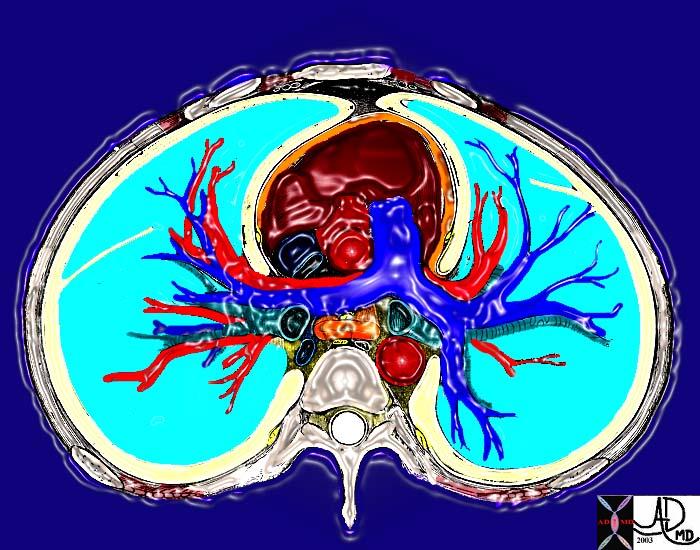
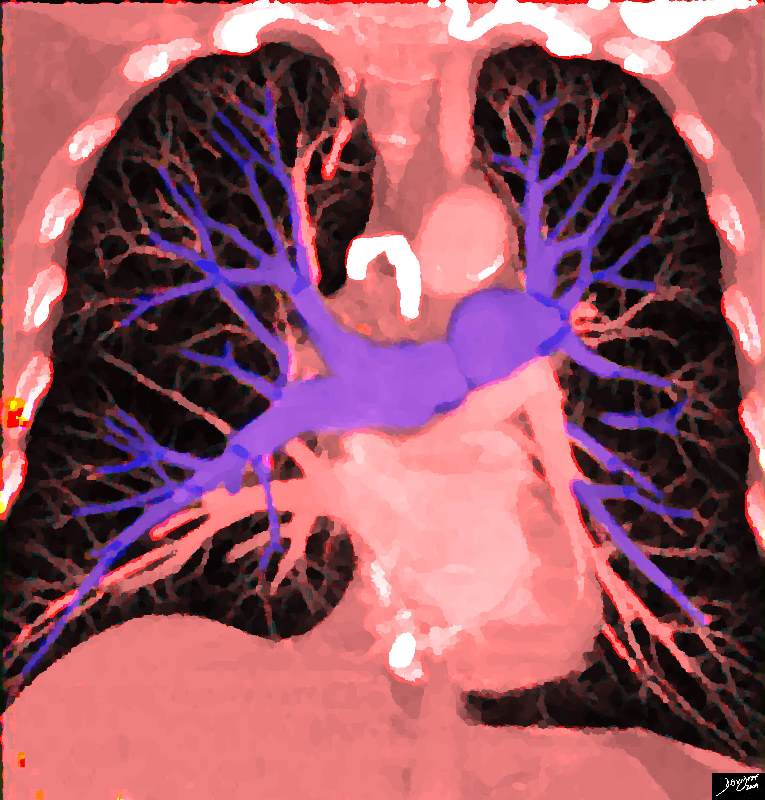
This cross sectional drawing shows the pulmonary artery in royal blue, pulmonary veins in red and the bronchi in teal. At the most central portion of each hilum there are usually 2 veins, one artery and one bronchus. This is because the length of the bronchus and artery prior to division is relatively long, while the confluence of the veins is close to the entrance into the left atrium. Thus the superior veins from the upper lobes are anterior and the veins to the inferior lobes are posterior. Courtesy Ashley Davidoff MD TheCommonVein.net 31592
Applied Anatomy
The distinction between the arteries and veins on plain film examination is often difficult. At the level of the hilum, it is a little easier since the LPA is superior to the more easily identified left bronchus and the RPA lies under the similarly easily identified right bronchus. The confluence of the veins into the LA is always inferior to the pulmonary artery.
As we proceed beyond the hilum the artery can be identified, as long as its low-density air filled bronchus buddy is with it.

This image shows the arteriole (royal blue) and the bronchiole (teal) travelling side by side bith of equal size. Ashley Davidoff MD TheCommonVein.net 42440b05
As the structures move more peripherally the bronchioles get more difficult to see and the distinction between artery and vein becomes difficult. On CT, the same principles hold, but an added feature of the difference in branching angles of the vessels sometimes is helpful. Arteries usually branch at acute angles, and veins branch at 90° angle.
In the lower lung fields the veins are horizontal as they course toward the left atrium while the arteries have a more vertical course
Pulmonary hypertension is characterized by enlarging arteries. The margins of the main arteries are usually quite distinct on the plain film. The lower lobe arteries should not measure more than 16mms in the male and more than 14mms in the femaleThey become blurred when there is interstitial edema, most commonly caused by heart failure.
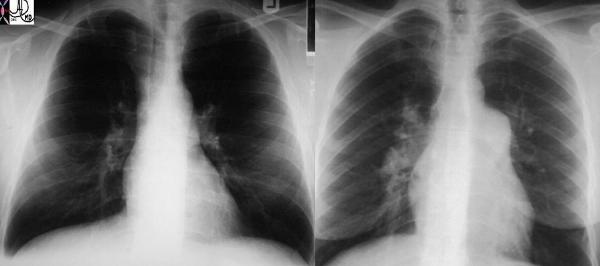
These two P-A chest X-rays show a normal cardio-mediastinal silhouette on the left and an abnormally enlarged MPA and RPA on the right in this patient with pulmonary hypertension.
Ashley Davidoff MD TheCommonVein.net 22089
Two of the common diseases of the pulmonary arteries include pulmonary embolism and pulmonary arterial hypertension. Pulmonary embolism has been an elusive diagnosis in the past and had been a commonly life threatening condition that was frequently missed. The advent of CT angiography with multidetector scanners has made the diagnosis much easier.
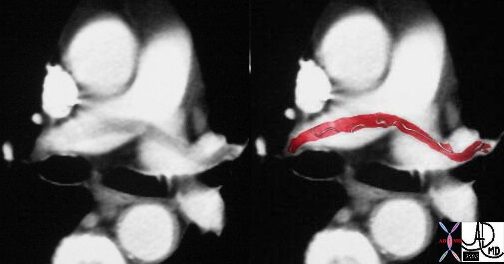
This case of a saddle embolus shows a thrombus sitting astride the left and right pulmonary arteries. Contemporary CTA is able to identify emboli in secondary and tertiary branches just as well. CTA has become the gold standard and study of choice in the patient with chest pain or acute desaturation with suspected PE.
Ashley Davidoff MD TheCommonVein.net 30008c
Pulmonary hypertension may be idiopathic, due to underlying chronic lung disease, or due to the less common congenital heart disease. In congenital heart disease pulmonary arterial abnormalities are common. In left to right shunts, including ASD, VSD, and PDA, there is an increase in flow in the pulmonary arteries due to the left to right shunt, with resulting increase in pulmonary pressure.
Transposition of the great vessels is a congenital abnormality where there is abnormal connection between the great vessels and their ventricles. In D transposition the MPA arises from the LV while the aorta arises from the RV. Transposition is a rather odd situation. Consider the travels of a deoxygenated red blood cell (rbc) returning from the calf muscle via the IVC. It will find itself first in the right atrium then in the right ventricle and then in the aorta, finally landing back in the systemic arterial circulation without oxygen replenishment. It will continue to go round a round becoming more and more desaturated, and without replenishment the tissues will be starved of life sustaining oxygen. This is a non viable situation. A rbc returning with oxygen from the lungs will enter the LA, then the LV, and will go back into the lungs via the MPA. The oxygen it carries gets delivered back to the alveoli and there will be little additional transfer of oxygen since the blood is fully saturated. i.e. all dressed up with oxygen and nowhere to go. Thus for life to be sustained, there has to be a shunt where the two circulations can mix. This may be in the form of a patent ductus arteriosus, VSD or ASD.
Early diagnosis and corrective surgical switching of the great vessels so that they can appropriately connected is key to survival.
Another serious anomaly is a variety of hypoplastic growth abnormalities of the pulmonary outflow tract ranging from stenosis to total atresia.
The other arterial circulation to the lungs – the bronchial circulation, can also be the source of disease. In chronic disease states such as cystic fibrosis, and bronchiectasis for example, chronic increase flow due to the inflammation and infection occurs, and the combination of an infected and friable mucosa with enlarged arteries, is a cause for hemoptysis. The treatment of choice for recurrent hemoptysis is embolization of the bronchial arteries.
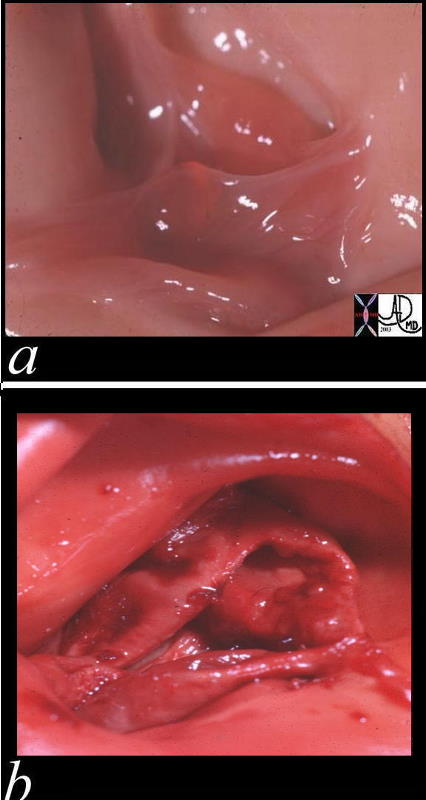
These two pathological specimens of the pulmonary valve show the delicate leaflets of the normal valve (a) in comparison to the thickened leaflets of the bicuspid pulmonary valve Courtesy Ashley Davidoff MD 00272c01.800
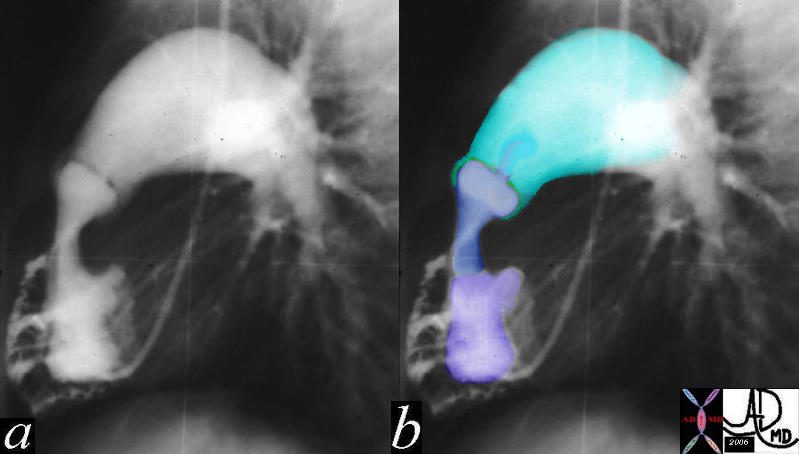
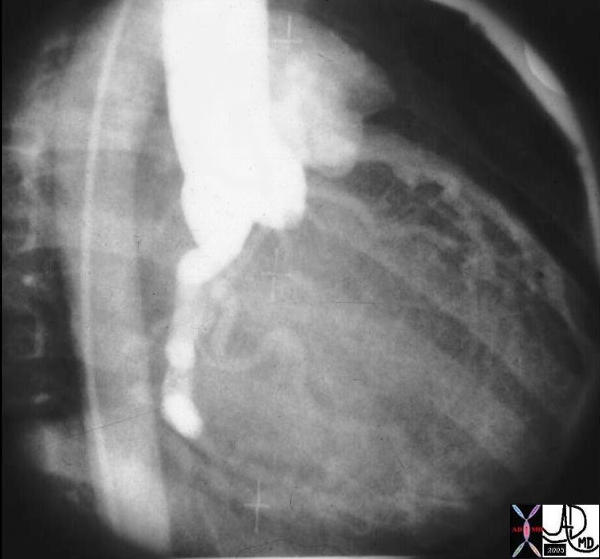
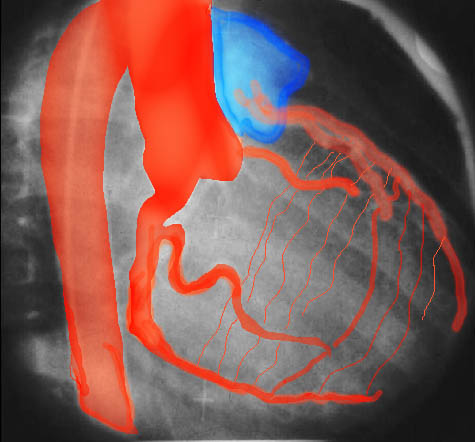
The lateral projection of this right ventricular angiogram reveals a case of severe pulmonary stenosis. The catheter enters the RV from the RA via the SVC. The RV inflow tract (purple) is hypoplastic. The vessels emanating and the-RV inflow are coronary arteries that are filling in retrograde fashion are due to the supra-systemic pressures in the RV indicating severe pulmonary stenosis with pressures in the RV that probably exceed 100mmhg. The infundibulum (right ventricular out flow tract (blue) is slightly narrow since it is hyperdynamic in an attempt to force the blood through the stenotic valve. The valve (green) is doming into the PA due the severe narrowing. The narrowing causes turbulence which causes the post stenotic dilatation.15036c01
Ashley Davidoff MD TheCommonVein.net
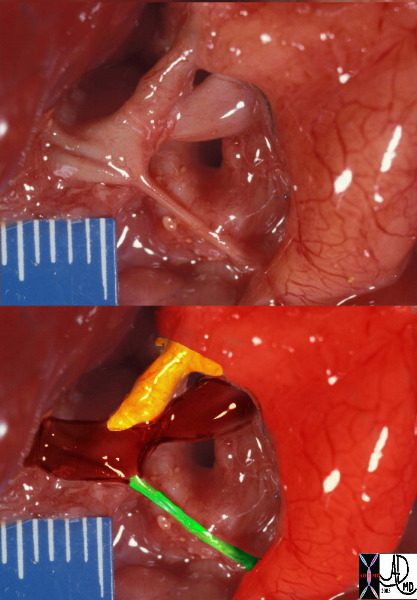
This is a post mortem specimen of a baby who died with pulmonary atresia. The atretic MPA overlayed in green in the lower image is connected to patrent branch pulmonary arteries in maroon, which are fed by a patent ductus arteriosus (yellow) arising from a anteriorly positioned left sided aorta, (red overlay) compatible with a diagnosis of transposition of the graet vessels – LTGA A.
Ashley Davidoff MD TheCommonVein.net 32627bC02
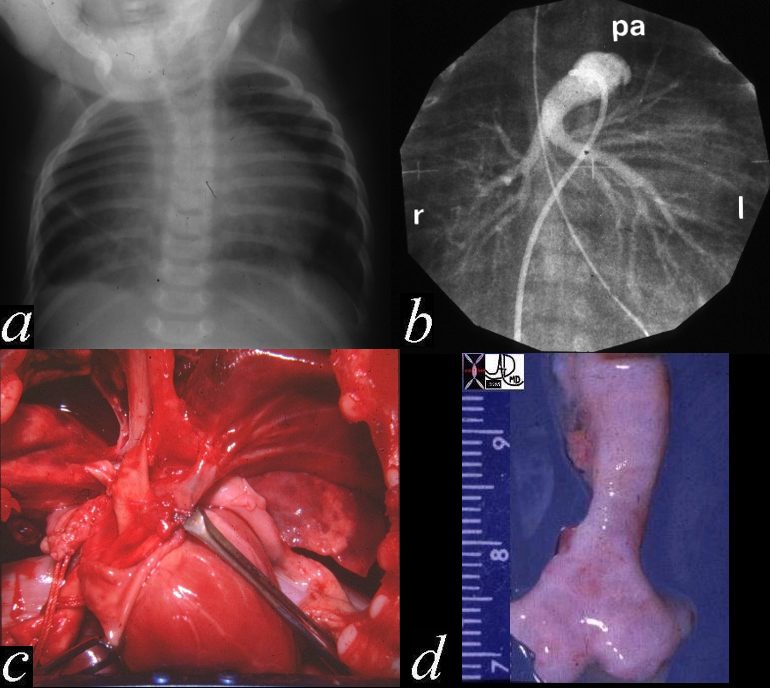
This autopsy is from a neonate who had respiratory difficulty at birth and showed a hyperinflated right lung with secondary leftward mediastinal shift. (a) A pulmonary angiogram showed the right pulmonary artery arising from the left PA rather than from the MPA (b) The gross in situ pathology shows the RPA coursing behind the trachea (c), while the last image (d) shows the narrowing of the left distal trachea. Histologically there was tracheomalacia secondary to the pressure effects of the LPA n the right side of the trachea causing right died bronchial obstruction with air trapping in the right lung. 01533c02
Ashley Davidoff MD TheCommonVein.net
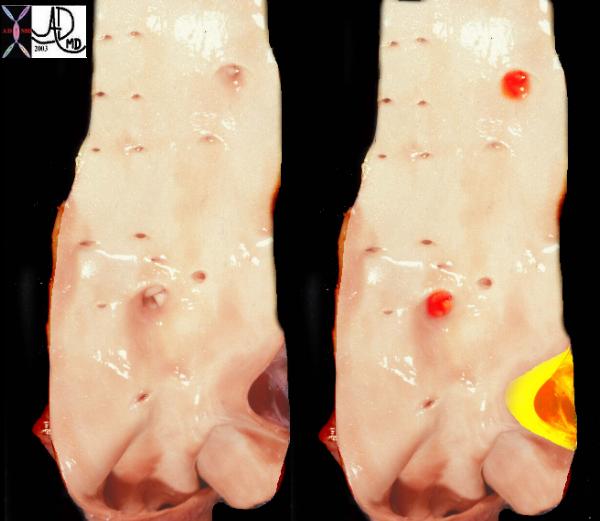
This is a post mortem specimen of the aorta of a patient with pulmonary atresia and bronchial collaterals. Overlaid in red are the enlarged orifices of the origins of the bronchial arteries. In yellow is the entrance of the PDA (patent ductus arteriosus) to the aorta Note in addition the normal appearing shiny appearance of the neonatal intima.
Ashley Davidoff MD TheCommonVein.net 32628c
Anomalous origin of the left Coronary artery from the Main Pulmonary Artery

Ashley Davidoff MD
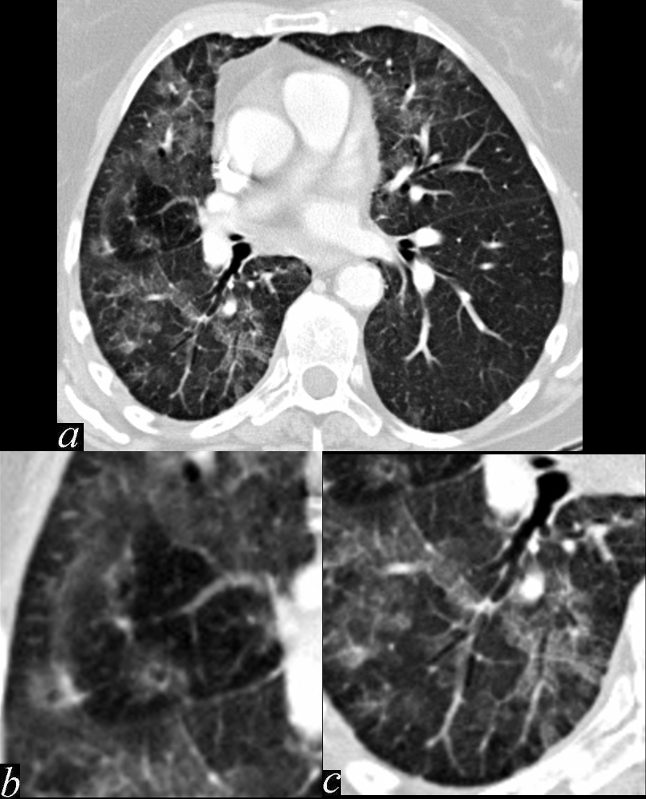
This series of images shows some subtle changes that reflect the local control of blood flow to a small segment of the right middle lobe. Note that in image a, there is a small area of increased lucency (blacker) in the right lung just lateral to the vessels of the right hilum. This region is highlighted in b. Note also that in b, the rapid diminution of the size of the blood vessel to that subsegment when compared to the size change of the vessels in the image in c. The lucent appearance of the lung suggests air trapping and the vasoconstriction reflects decreased perfusion – ie with decreased ventilation there is an associated consequent associated decrease in perfusion.
47170c01.800 broncho-centric inflammation lung bronchovascular bundle chest inflammation peribronchial halo air trapping mosaic perfusion ground glass changes alveolar change air bronchogram acute bronchovascular inflammation ddx allergic collagen vascular disease infection CTscan
Ashley Davidoff MD TheCommonVein.net
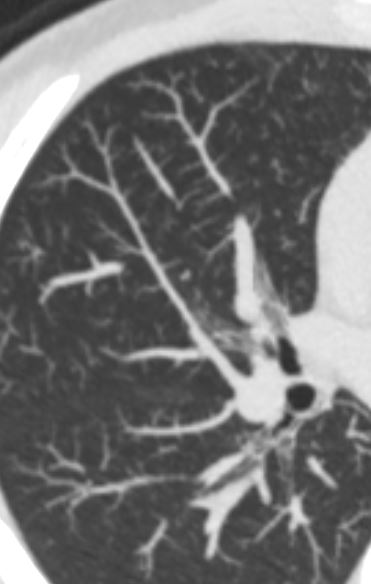
Encasement by Squamous Cell Carcinoma
Large Central Mass with Obstruction of the Pulmonary Vein and Encasement of the Arteries – Squamous Cell Carcinoma

Ashley Davidoff MD TheCommonVein.net occluded-pulm-vein-005
Ashley Davidoff MD TheCommonVein.net occluded-pulm-vein-001
Ashley Davidoff MD TheCommonVein.net occluded-pulm-vein-001
Links and References
Marini, T.J et al Pictorial review of the pulmonary vasculature: from arteries to veins Insights Imaging. 2018 Dec; 9(6): 971–987.