- Buzzwords
- serious infection,
- may be systemic
- immunocompromised
- Invasive Aspergillosis:
- A severe fungal infection caused by Aspergillus species.
- Primarily affects individuals with weakened immune systems,
- transplant recipients,
- chemotherapy patients, and those with
- HIV/AIDS.
- Also
- chronic obstructive pulmonary disease (COPD)
- Symptoms:
- Fever, often unresponsive to antibiotics.
- Chest pain.
- Cough with or without blood.
- Shortness of breath.
- Fatigue.
- DiagnosisCT scans
- Halo Sign:
- An early sign often seen in neutropenic patients.
- Presents as a central area of lung attenuation (ground-glass opacity) surrounded by a rim of ground glass.
- Indicates hemorrhage and edema around the infected area.
- Halo Sign:
Halo Sign
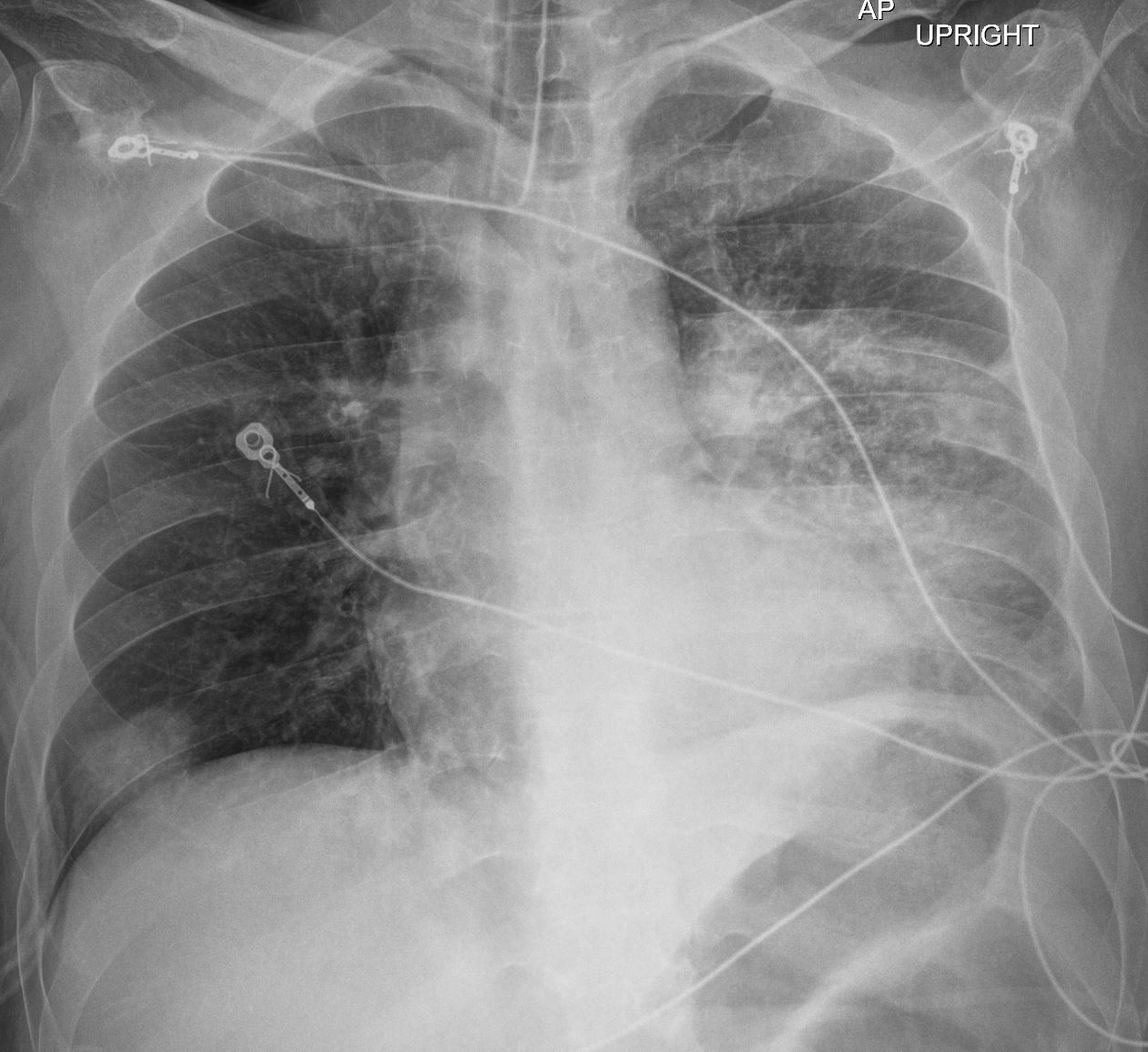
The Frontal CXR shows a rapidly progressive interstitial infiltrate in the left upper lobe with a focal subsegmental infiltrate in the right lower lobe Diagnosis Aspergillus Infection
Ashley Davidoff TheCommonVein.net 219Lu-001b

The coronal CT scan shows a rapidly progressive interstitial infiltrate in the left upper lobe showing features of a halo sign There is evidence of bronchial wall thickening.
Diagnosis Aspergillus Infection
Ashley Davidoff TheCommonVein.net 219Lu-002
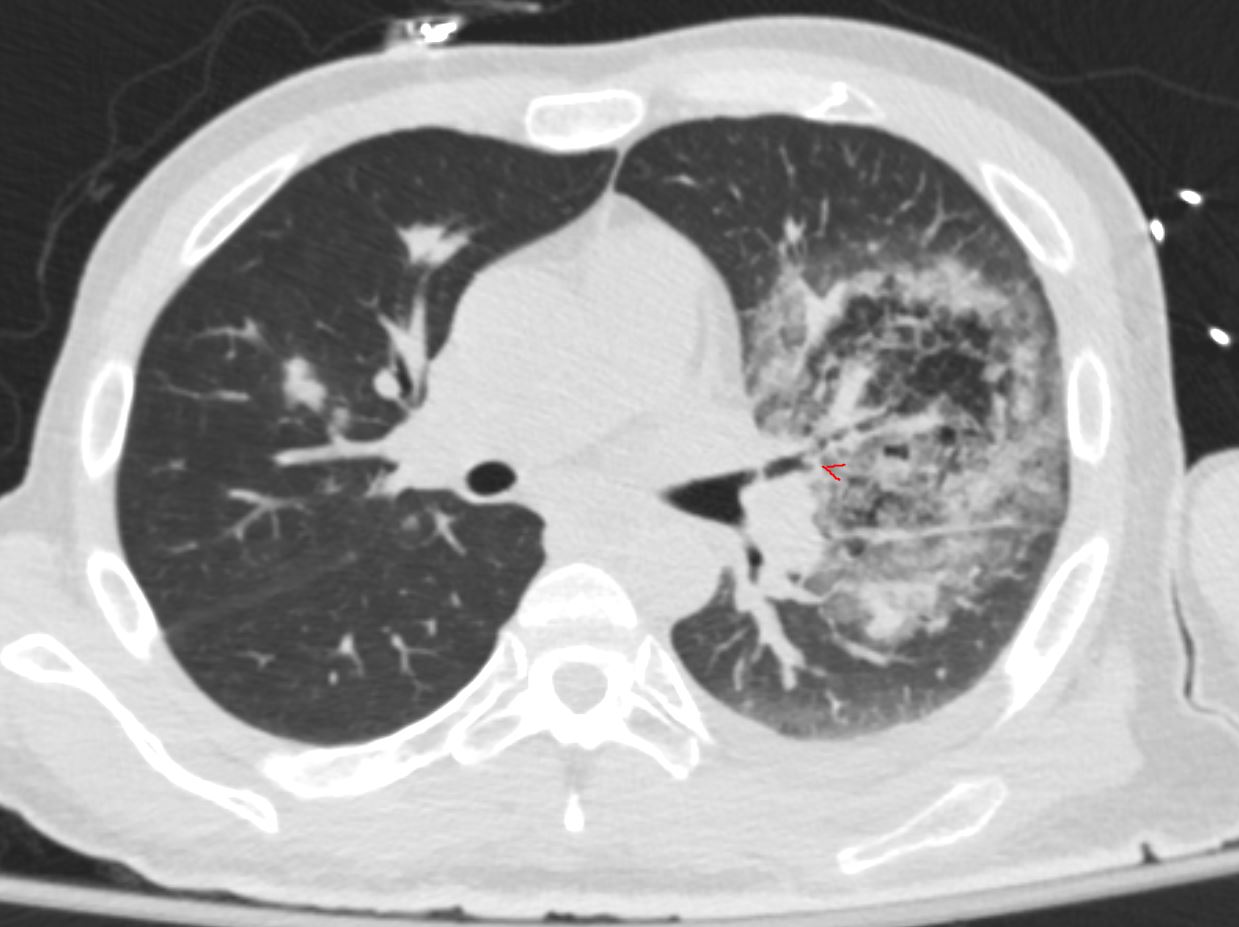
The coronal CT scan shows a rapidly progressive interstitial infiltrate in the left upper lobe showing features of a halo sign There is evidence of bronchial wall thickening.
Diagnosis Aspergillus Infection
Ashley Davidoff TheCommonVein.net 219Lu-008
-
- Reversed Halo Sign:
Diagnosis Aspergillus Infection
Ashley Davidoff TheCommonVein.net219Lu-014
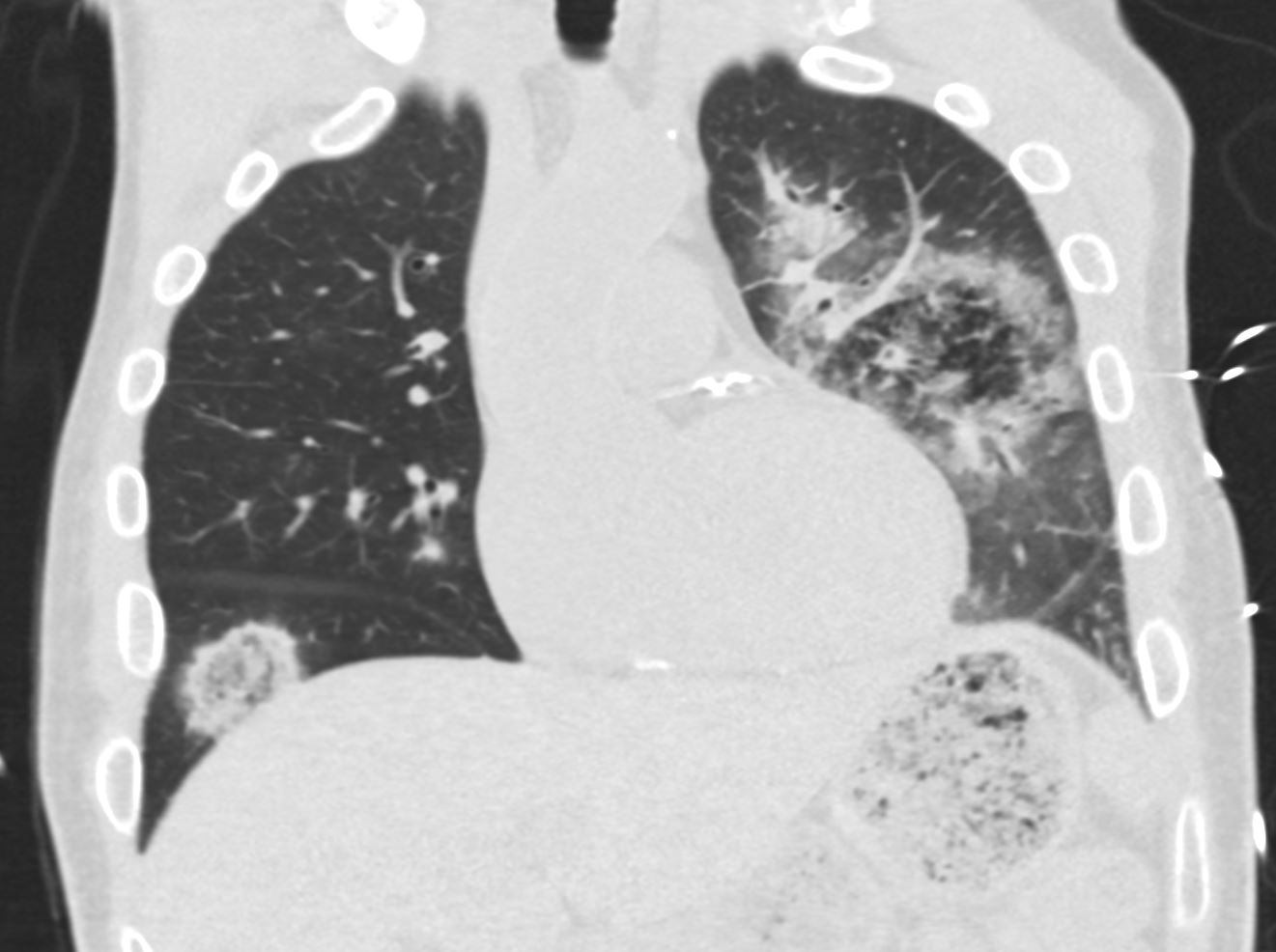
The coronal CT scan shows a rapidly progressive interstitial infiltrate in the left upper lobe (halo sign) with a focal subsegmental infiltrate in the right lower lobe, showing features of a reversed halo sign (Atoll sign) There is evidence of bronchial wall thickening.
Diagnosis Aspergillus Infection
Ashley Davidoff TheCommonVein.net 219Lu-004
-
- Nodules and Masses:
- As the infection progresses, nodules and masses can develop in the lung tissue.
- Nodules and Masses:
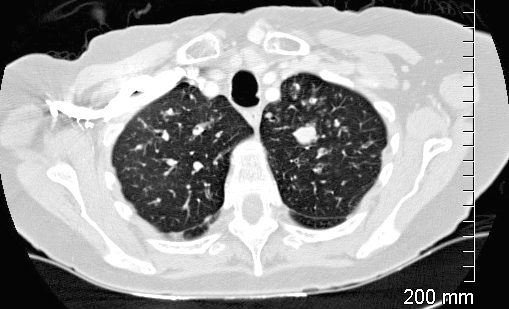
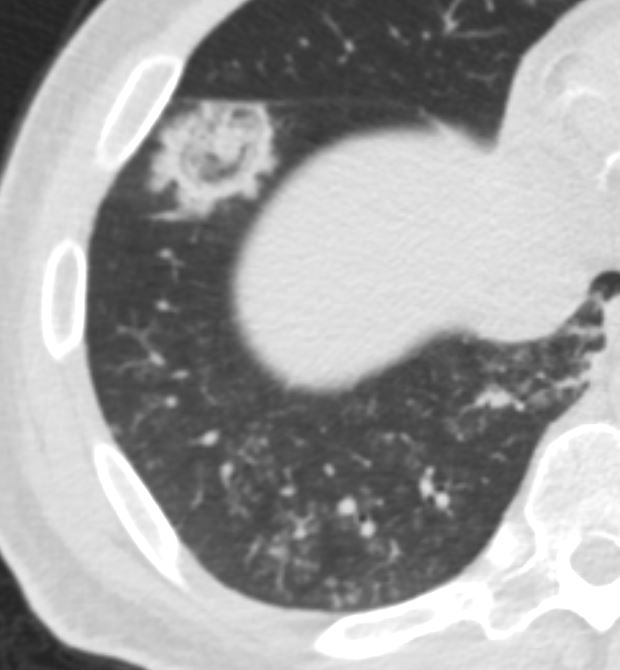
CT of the upper lobes show ground glass micronodules reminiscent of small airway disease
Impacted bronchus is noted in the left apex
Ashley Davidoff TheCommonVein.net 135123
Axial Ct scan focused on the right lung base shows ground glass micronodules revealing a combination of centrilobular nodules and tree in bud sign indicating small airway disease
Diagnosis Aspergillus Infection
Ashley Davidoff TheCommonVein.net 219Lu-015
-
-
- Irregular borders and variable enhancement patterns are typical.
- Nodules can cavitate, leading to the air crescent sign.
-
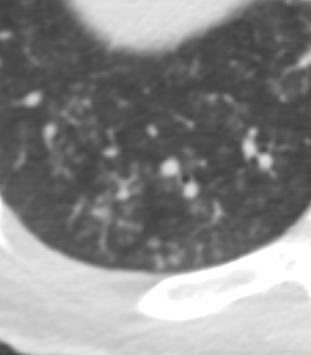
Air Crescent Sign
CT scan in the axial projection with the patient in the supine position shows a soft tissue mass in the right upper lung field with an anterior crescent shaped rim of air (blue arrowheads) anterior to the aspergillus fungus ball (a, magnified in b)
Since the fungus ball is movable, when the patient is placed in the the left decubitus position c and d), the fungus ball “sinks” to the dependent position and the air moves to the most superior position (blue arrowheads)
Ashley Davidoff TheCommonVein.net 78612a L
-
- Pneumonia
- Cavitation and Necrosis:
- Advanced invasive aspergillosis can lead to cavitation and necrosis of lung tissue.
- Cavities may contain fungal elements, blood, and debris.
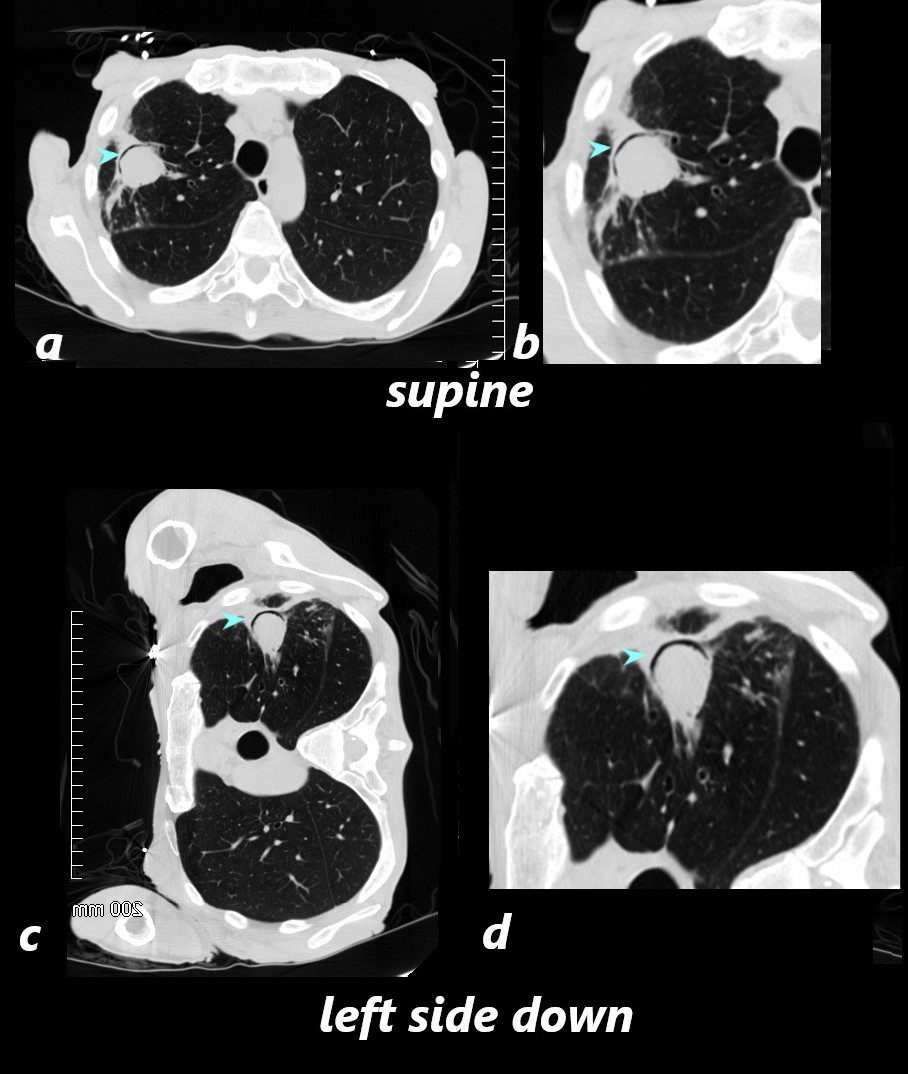
Cavitation and Necrosis
CXR and CT of a 54 year old male shows hyperinflation of the lungs, with large left apical cavity with aspergilloma and pneumonic consolidation and abscess formation in the apex of the right lung. These findings are consistent with chronic pulmonary aspergillosis
Ashley Davidoff TheCommonvein.net
- Angioinvasive Aspergillosis:
- subtype of invasive aspergillosis.
- refers to the tendency of the Aspergillus hyphae to
- invade and infiltrate blood vessels particularly the small
- causes
- vessel damage,
- thrombosis
- tissue infarction
Angioinvasive with Multiple Nodules in the Liver and Spleen
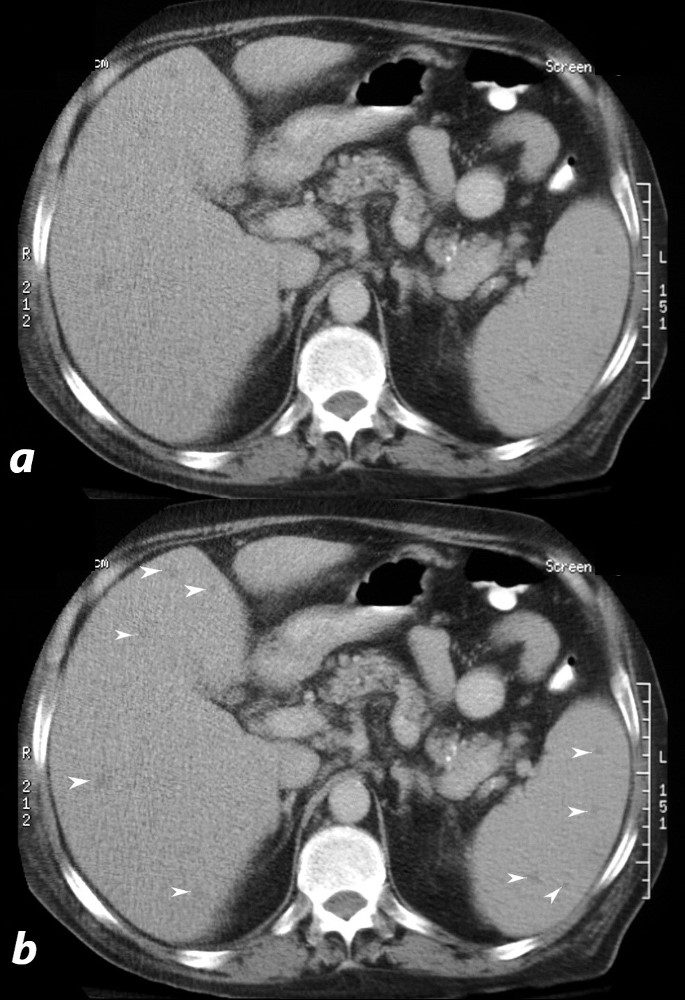
66 year malnourished immunodeficient male with right upper lobe aspergilloma in the lung
CT scan in the axial projection shows multiple ill defined nodules in the the liver and spleen (white arrowheads in b, suggesting fungal deposits in the clinical context
Ashley Davidoff TheCommonVein.net 20762
Angioinvasive Causing Splenic Infarction
Wedge Shaped Infarct in the Spleen
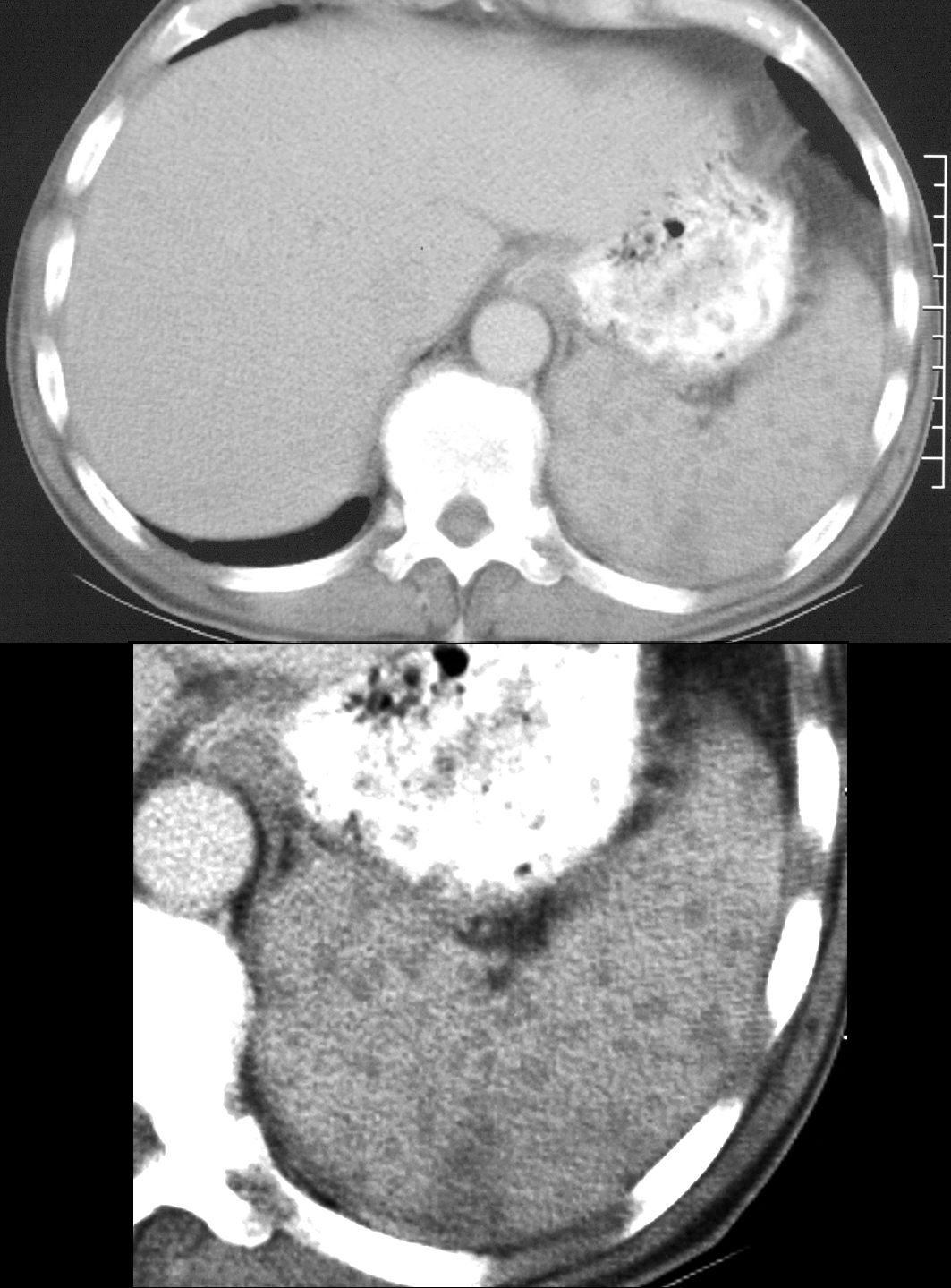
CT scan in the axial projection in an immune compromised host shows multiple sub cms nodules in the spleen with a wedge shaped peripheral defect A diagnosis of Aspergillus was confirmed and these findings are consistent with angioinvasive aspergillosis
Ashley Davidoff TheCommonVein.net 20758c
-
-
- Pleural Involvement:
- In severe cases, infection can extend to the pleura.
- Pleural effusion and pleural thickening may be observed.
- Distribution:
- Lesions are often multiple and can be bilateral.
- More commonly found in the upper lobes and periphery of the lungs.
- Pleural Involvement:
- Laboratory tests including blood cultures and biomarker tests (such as galactomannan or β-D-glucan).
-
- Treatment:
- Antifungal medications (voriconazole, isavuconazole, or other options based on susceptibility).
- Intravenous therapy followed by oral treatment.
- Close monitoring of drug levels and potential interactions, especially in patients on multiple medications.
- Prognosis:
- Mortality rates can be high, especially in severely immunocompromised individuals.
- Early diagnosis and prompt treatment are critical for better outcomes.
- Prognosis improves if underlying immune issues can be addressed.
- Prevention:
- Minimizing exposure to environmental mold and fungi, especially in healthcare settings.
- Taking appropriate precautions for individuals with weakened immune systems.
- Timely administration of antifungal prophylaxis in high-risk patients.
