The Common Vein Copyright 2012
- Buzz Words
- Alveolar destruction
- Loss of elasticity
Definition
- Emphysema is an inflammatory disease of the lung
- characterized
- alveolar and small vessels destruction with
- Loss of elasticity
- clinically characterised by
- shortness of breath, and other respiratory problems.
- characterized
- Caused mostly by
- smoking and sometimes by a
- inherited deficiency of a protein called
- alpha 1-antitrypsin (AAT).
- Results
- Structurally
- alveolar wall destruction
- decreased lung elasticity,
- architectural distortion of the capillary bed.
- Types
- Structurally
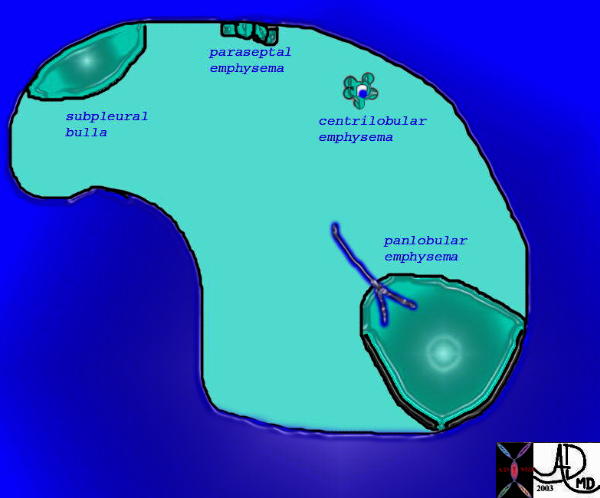
Types of Emphysema |
| This is a drawing showing the structural changes occuring in diseases that have confluens of the alveoli due to wall destruction which in its classical form is known as emphysema. In centrilobular emphysema the bronchovascular bundle is usually seen, surrounded by a rosette of expanded alveolar space. In panacinar emphysema the expanded spaces are generally larger.
Courtesy Ashley Davidoff MD. 32174 |
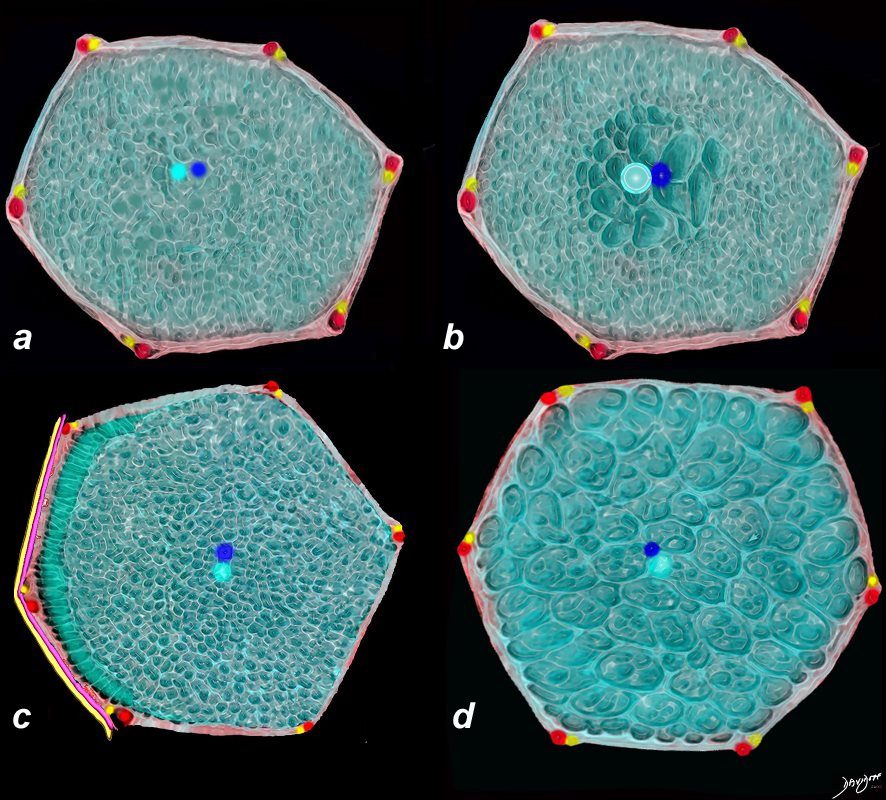
The diagram shows a normal secondary lobule of the lung(a) centrilobular emphysema (b) paraseptal emphysema ((c) and panlobular emphysema (d)
Ashley Davidoff MD The CommonVein.net
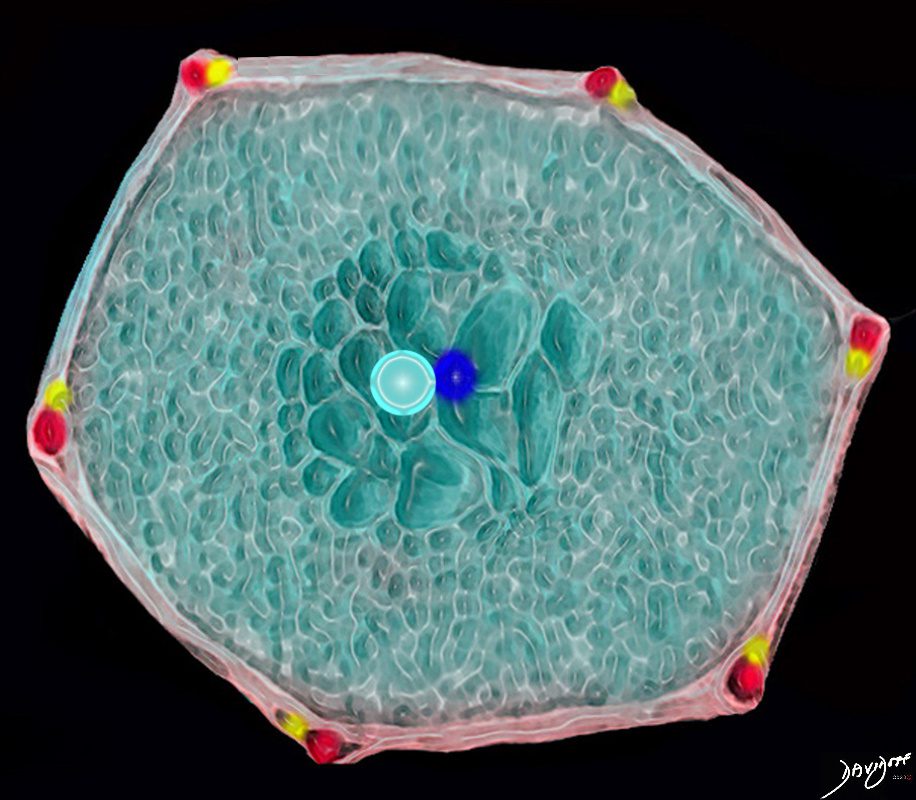
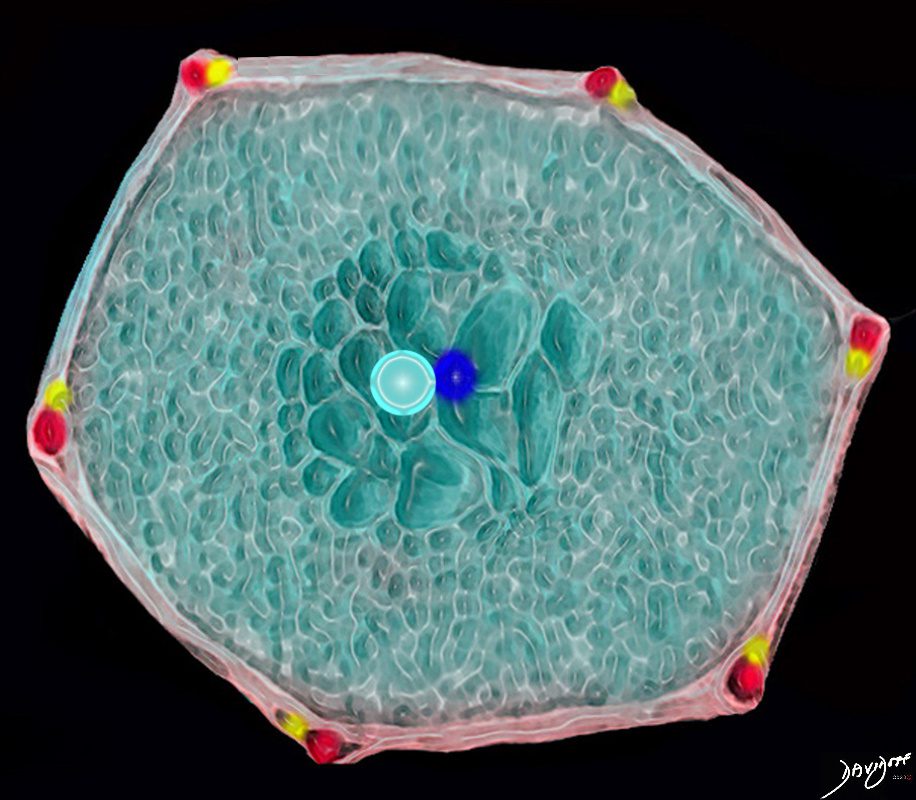
This drawing shows a secondary lobule with centrally located dilated airspaces starting with the respiratory bronchiole and extending to the proximal structures including the alveolar ducts, sacs and alveoli
Ashley Davidoff TheCommonVein.net
-
- Functionally
- Air trapping
- Functional distortion of the capillary bed.
- decreased gas exchange
- Clinically
- irritation
- coughing,
- wheezing,
- decreased function
- insufficient oxygen,
- shortness of breath,
- anxiety,
- weight loss,
- fatigue.
- irritation
- Functionally
- Diagnosed by
-
- pulmonary function tests,
- chest X-rays,
- oxygen level tests,
- pulmonary ventilation/perfusion scan, and
- chest CT scan.
-
- Treated by
-
- quitting smoking,
- bronchodilators,
- corticosteroids,
- diuretics
- antibiotics,
- low-flow oxygen,
- pulmonary rehabilitation,
- lung reduction.
- lung transplant
-
Etymology of emphysema
The word “emphysema” has its origins in ancient Greek. It comes from the Greek words “en” (meaning “in” or “within”) and “physema” (meaning “inflation” or “swelling”). In Greek medical terminology, “emphysema” referred to a condition characterized by the abnormal accumulation of air or gas within tissues or spaces of the body.
The term was used to describe various medical conditions where abnormal pockets of air or gas could form, leading to swelling and distension of tissues. Over time, the term became more specifically associated with a lung condition characterized by the permanent enlargement of airspaces within the lungs, resulting in difficulty breathing and reduced lung function. This condition is now commonly known as pulmonary emphysema.
The word “emphysema” was adopted into English and other languages from its Greek roots to describe this medical condition. The term has retained its meaning related to the abnormal accumulation of air within tissues, particularly within the context of lung diseases.
Normal Lung
Emphysema, bullous, subpleural –
magnified
Large, prominent subpleural bullae. Spontaneous pneumothorax often results from rupture of such lesions.
Ashley Davidoff MD



Large, prominent subpleural bullae. Spontaneous pneumothorax often results from rupture of such lesions.
Courtesy Yale Rosen MD
Ashley Davidoff MD
The cause of the disease is most commonly due to cigarette smoking and it results in enlargement of the distal airspaces, and loss of normal elastic recoil, with architectural and functional distortion of the capillary bed.
Structurally the disease is characterized by progressive expansion of the acinus without fibrosis, loss of functioning surface area, and functionally progressive difficulty with oxygenation due to disproportionate decrease in blood flow, and an overall decrease in functional surface area.
Secondary changes are characterized by a decreasing cardiac output, hyperventilation, and eventually pulmonary cachexia
Clinically the patient presents in middle age and older, as a barrel chested “pink-puffer, breathing often with pursed lips, with insidious and unrelenting dyspnea.
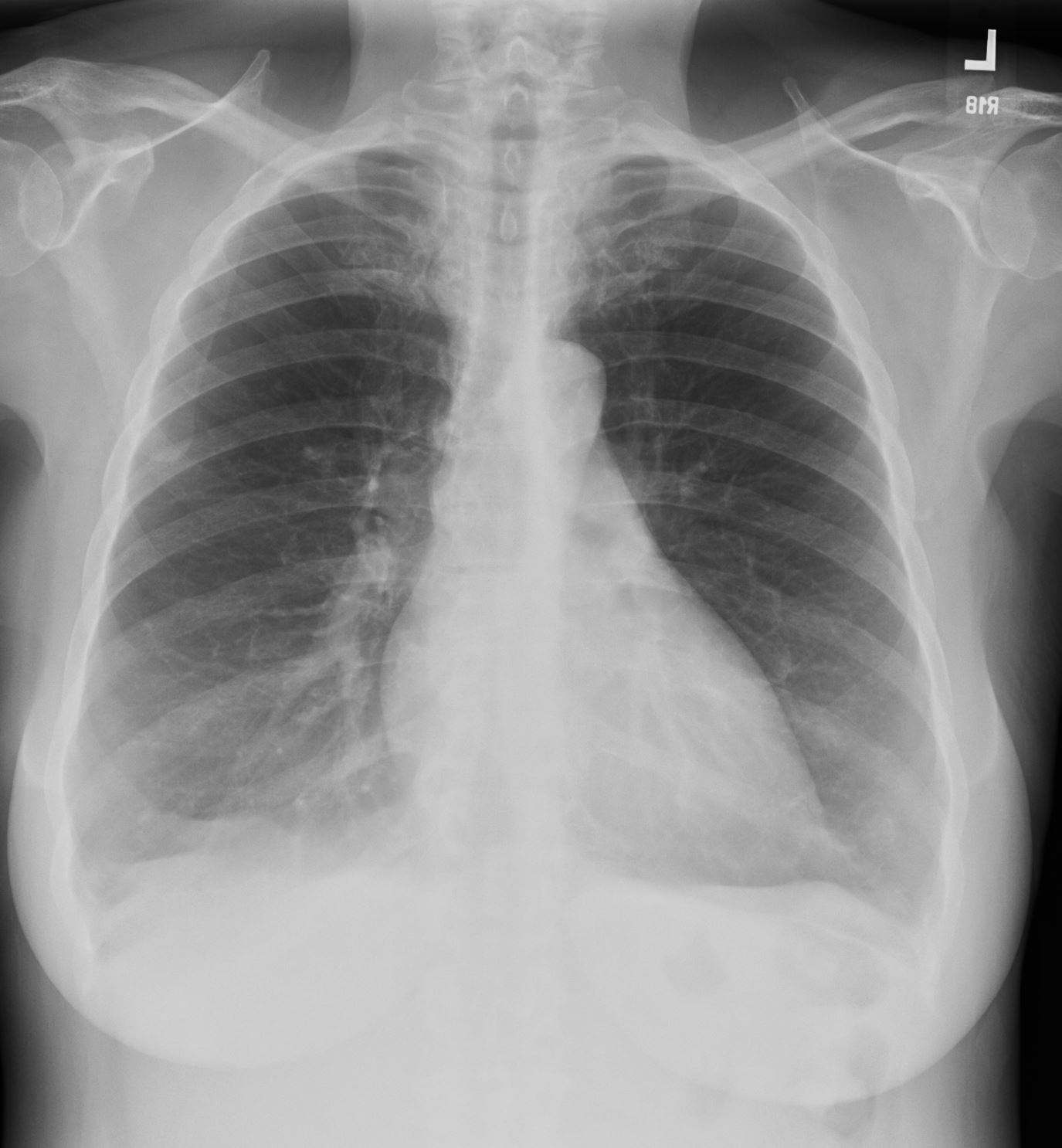
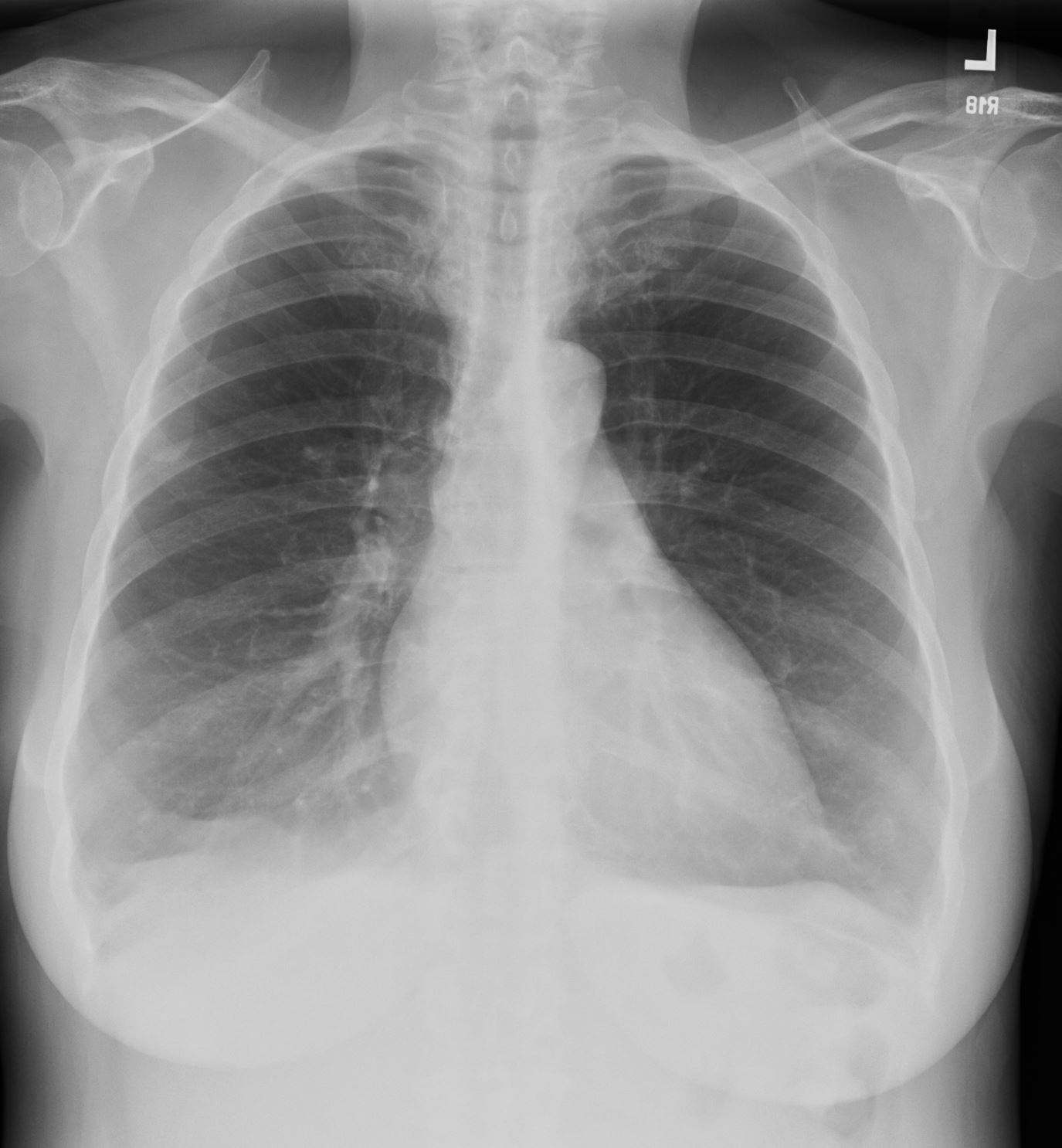
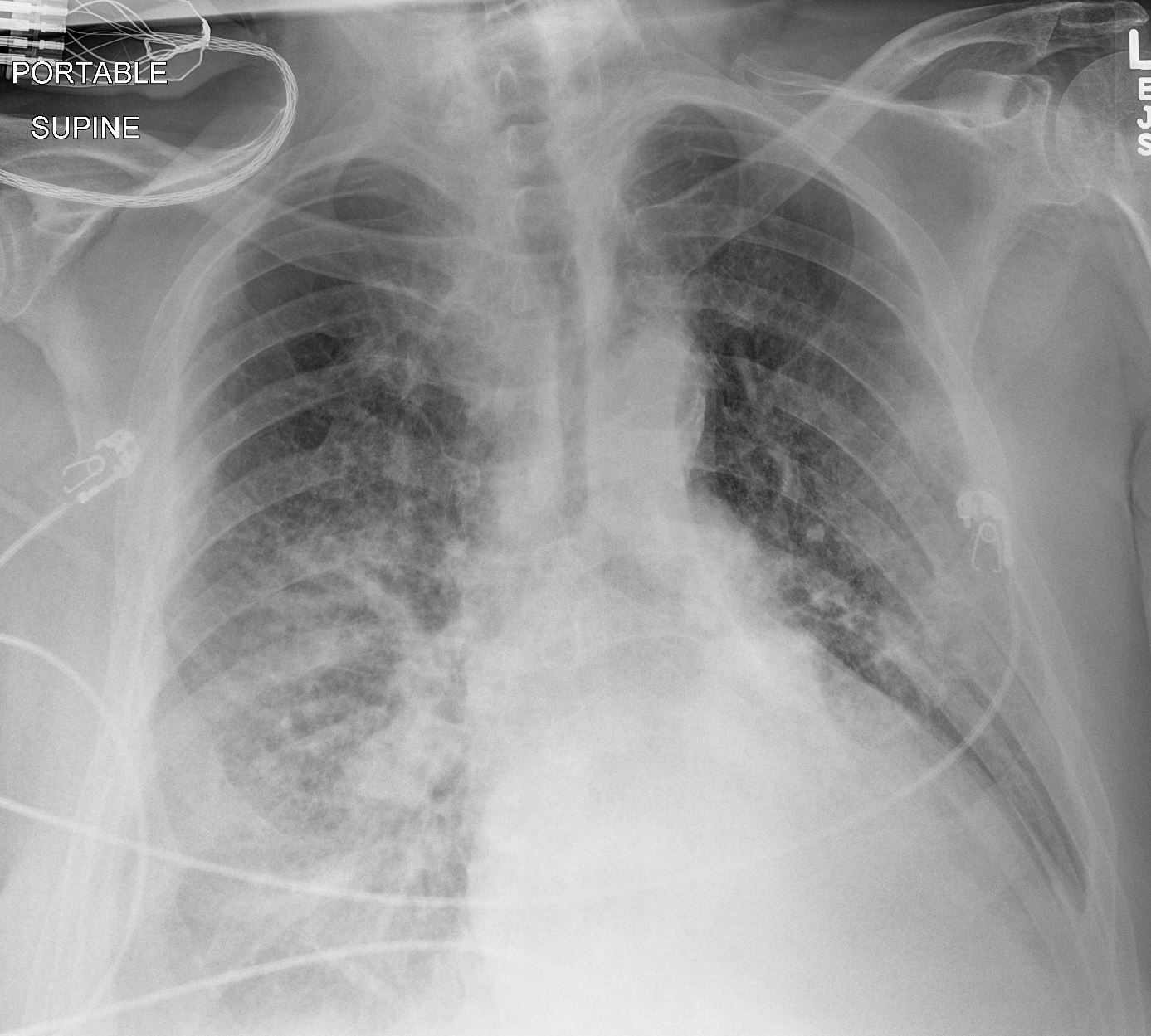
From a diagnostic standpoint the CXR shows hyperinflated lungs, with propensity for the upper lobes, often with flattened diaphragms and a pectus carinatum.
PFT’s show a reduction in the maximal expiratory flow during forced exhalation. (decreased FEV1)
The mainstays of therapy are bronchodilators, diuretics, corticosteroids, antibiotics, low-flow oxygen, pulmonary rehabilitation.
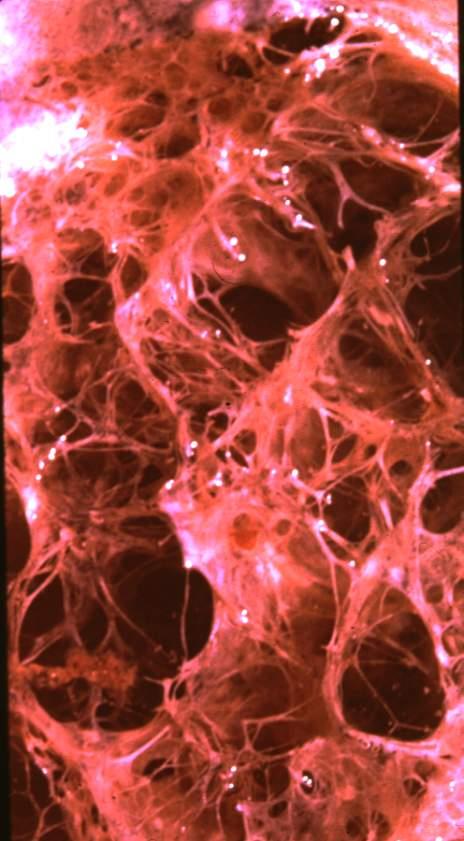
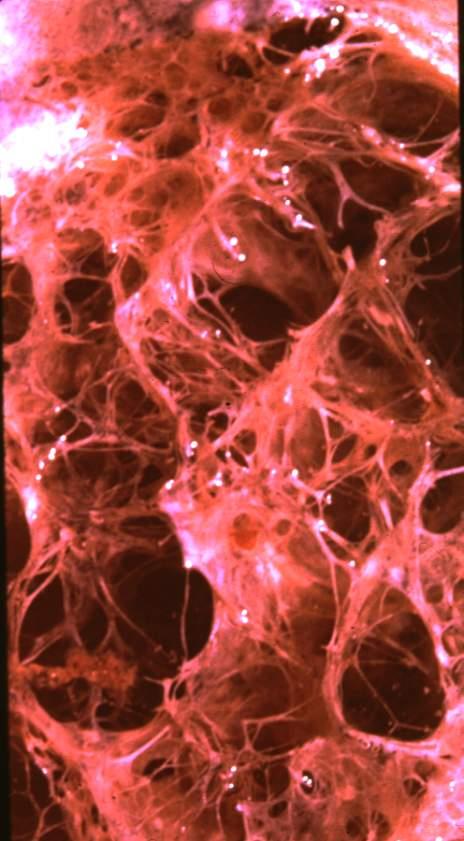
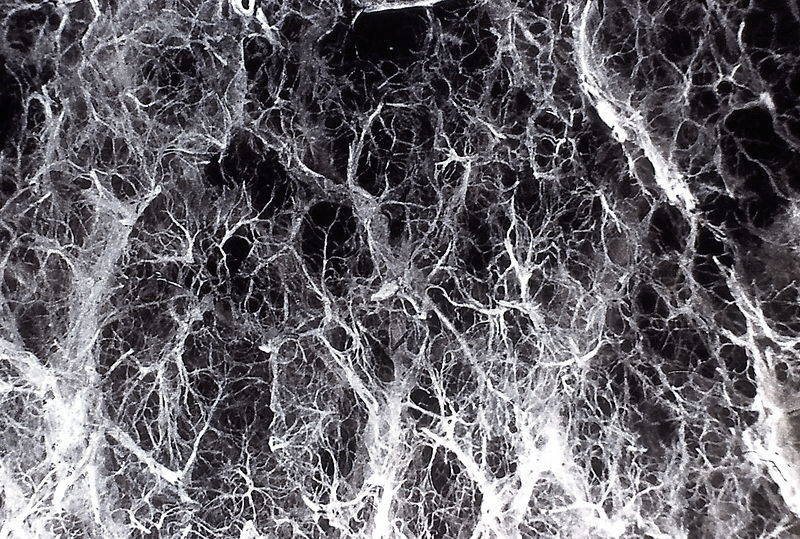
Principles
The lungs feel and act like a sponge. Sponges are functional and efficient in absorbing water by virtue of the elastic properties of the innumerable small holes or cavities in the matrix. For the given surface area of these small holes, the elastic recoil and capillary action is sufficiently strong and cohesive for the sponge to absorb effectively. If the holes are made bigger, then both the elastic properties and the capillary action are relatively diminished or lost and effectiveness to absorb and empty water is lost. In emphysema, destruction of the walls leads to a bigger acini and loss of elasticity as well as the capillary action. Movement of air is inefficient and excess air hangs around the distended alveoli without moving. The fewer and the bigger the alveoli, the less effectively they perform.
Loss of Structural Integrity
Break down of the alveolar walls leads to confluent expansion of the acinar complex,, and a reduction of total surface area. This results in destruction the efficient capillary network surrounding the alveoli and therefore a progressive mismatch of ventilation and perfusion. Most importantly loss of the elastic recoil results in the passive ability of the lungs to move air in and out of the alveoli, and hence a static column builds.
The lungs feel and act like a sponge. Sponges are functional and efficient in absorbing water by virtue of the elastic properties of the innumerable small holes or cavities in the matrix. For the given surface area of these small holes, the elastic recoil and capillary action is sufficiently strong and cohesive for the sponge to absorb effectively. If the holes are made bigger, then both the elastic properties and the capillary action are relatively diminished or lost and effectiveness to absorb and empty water is lost. In emphysema, destruction of the walls leads to a bigger acini and loss of elasticity as well as the capillary action. Movement of air is inefficient and exces air hangs around the distended alveoli without moving. The fewer and the bigger the alveoli, the less effectively they perform.


Ashley Davidoff MD
Ashley Davidoff MD
Ashley Davidoff MD
Protease – Antiprotease Mechanisms
The protease-antiprotease theory holds that alveolar wall destruction results from an imbalance between proteases (mainly elastase) and antiproteases in the lung
the protease-antiprotease mechanism. …. evolve this concept
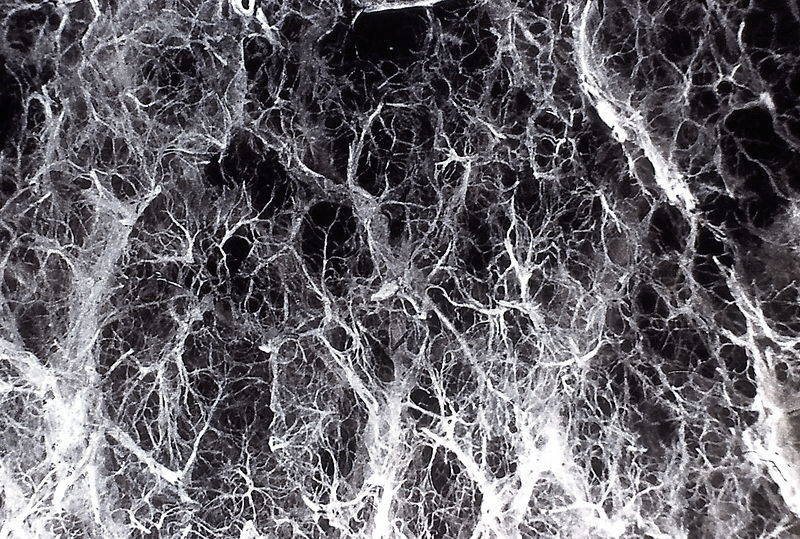
  Normal Lung |
|
Normal sponge like character of the lung Courtesy Ashley Davidoff MD. 32300d |
Classification
There are four major types: (1) centrilobular, (2) panacinar, (3) paraseptal, and whether the emphysema is centrilobular or panacinar.
Clinical management is independent on whether the emphysema is centrilobular or panacinar.
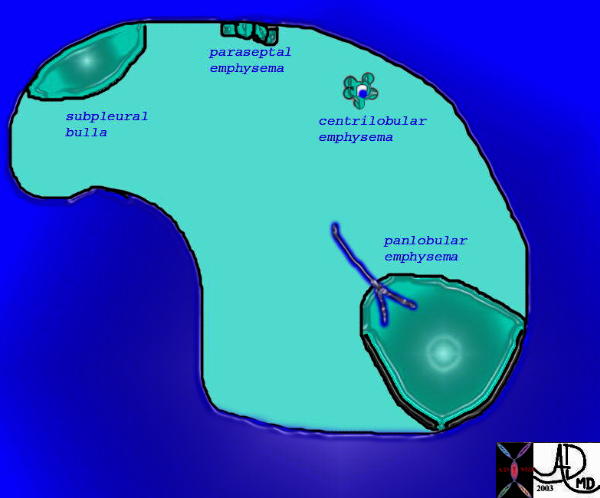 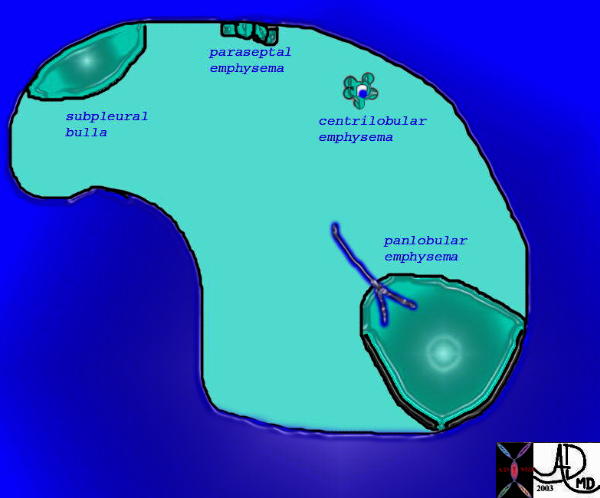 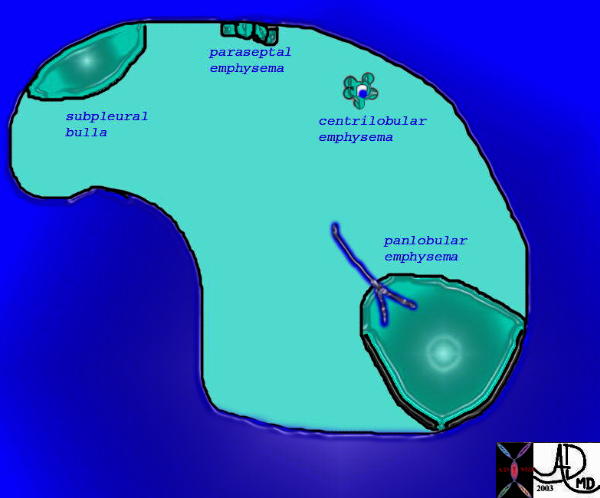 Types of Emphysema |
| This is a drawing showing the structural changes occuring in diseases that have confluens of the alveoli due to wall destruction which in its classical form is known as emphysema. In centrilobular emphysema the bronchovascular bundle is usually seen, surrounded by a rosette of expanded alveolar space. In panacinar emphysema the expanded spaces are generally larger.
Courtesy Ashley Davidoff MD. 32174 |
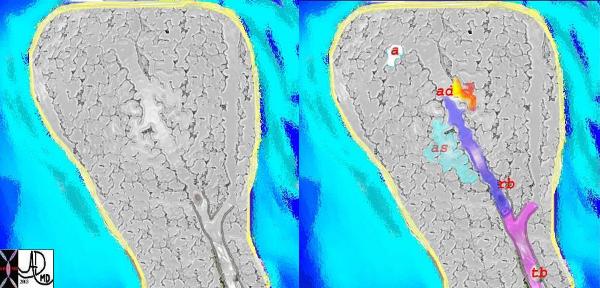 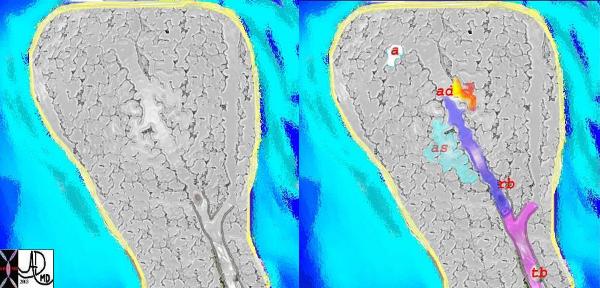 Secondary Lobule |
|
An artistic impression of a normal acinus with terminal bronchiole, (tb in pink) respiratory bronchiole, (rb dark blue) alveolar duct (ad in yellow/orange) and an alveolar sac (as – in teal) All the alveoli are in gray with a single exemplified (a in white) The interlobular septum is in yelow. Courtesy Ashley Davidoff MD 32652c |
Centrilobular Emphysema
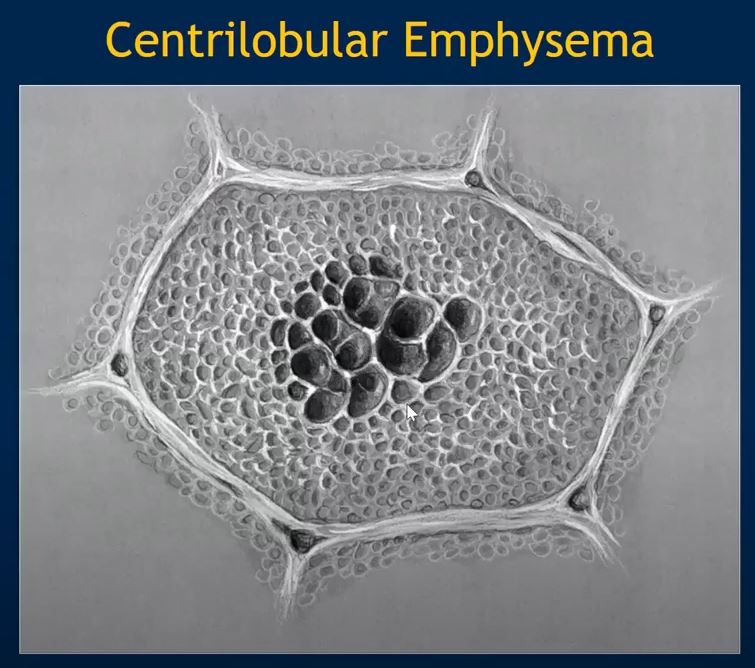
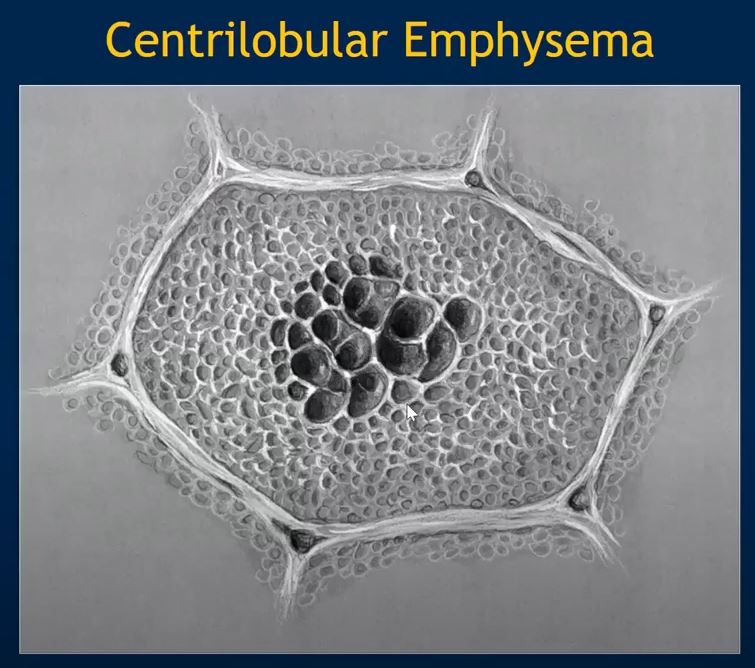
  Normal and centrilobular Emphysema |
|
An artistic interpretation of centrilobular emphysema. The first image is the normal, and the second shows in green, the characteristic proximal dilatation of the respiratory bronchiole, (rb) with relative sparing of the distal part of the acinus. Courtesy Ashley Davidoff MD. 32645f |
Flattened and Partially Inverted
Ashley Davidoff MD TheCommonvein.net


Flattened and Partially Inverted
Ashley Davidoff MD TheCommonvein.net


Flattened and Partially Inverted
Ashley Davidoff MD TheCommonvein.net
Ashley Davidoff MD
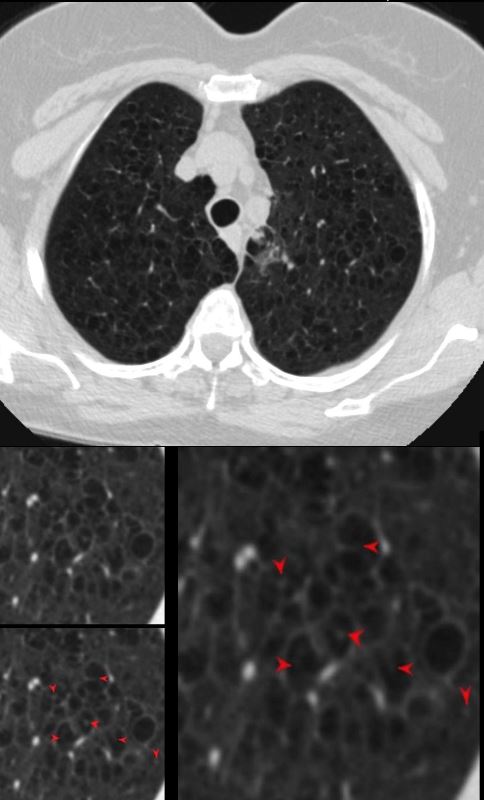
Centrilobular Emphysema with Honeycomb Lung Disease
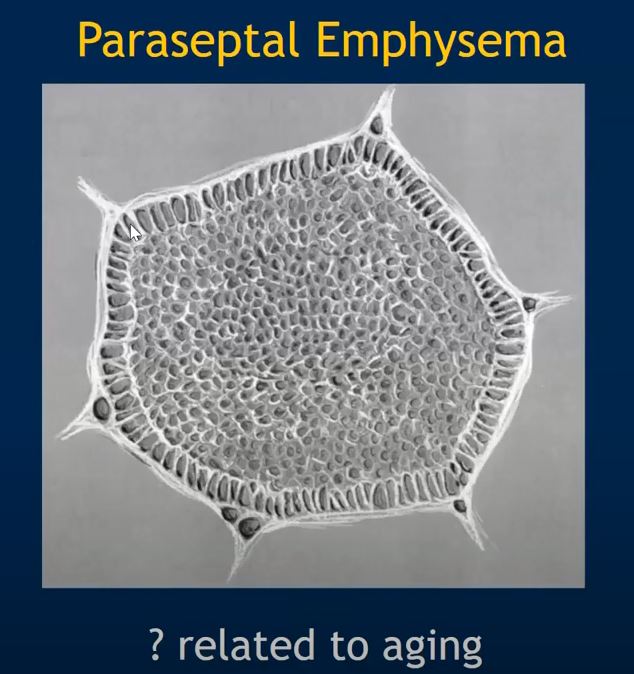
Paraseptal Emphysema
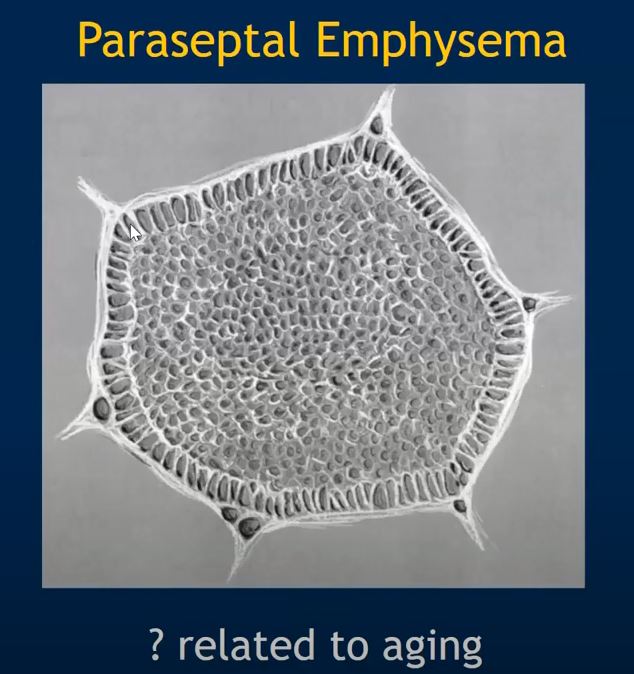



Large, prominent subpleural bullae. Spontaneous pneumothorax often results from rupture of such lesions.
Courtesy Yale Rosen MD


Ashley Davidoff MD
Panlobular Emphysema
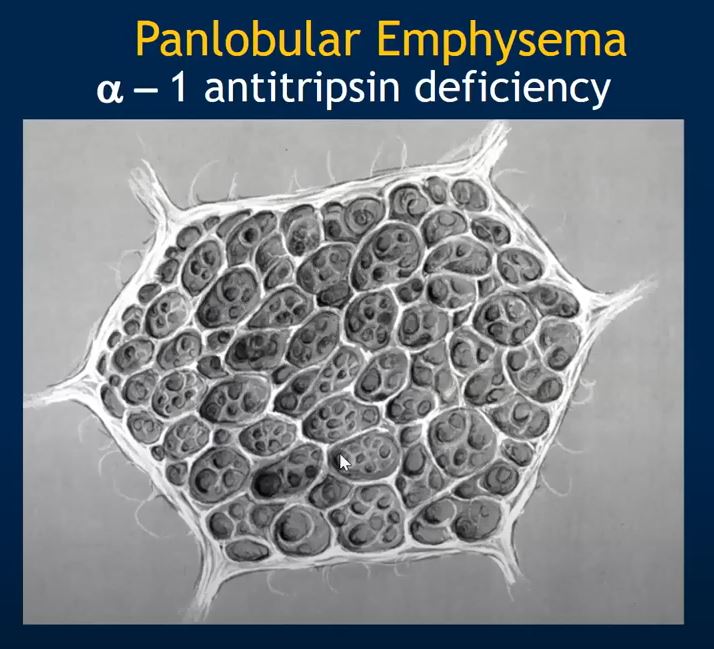
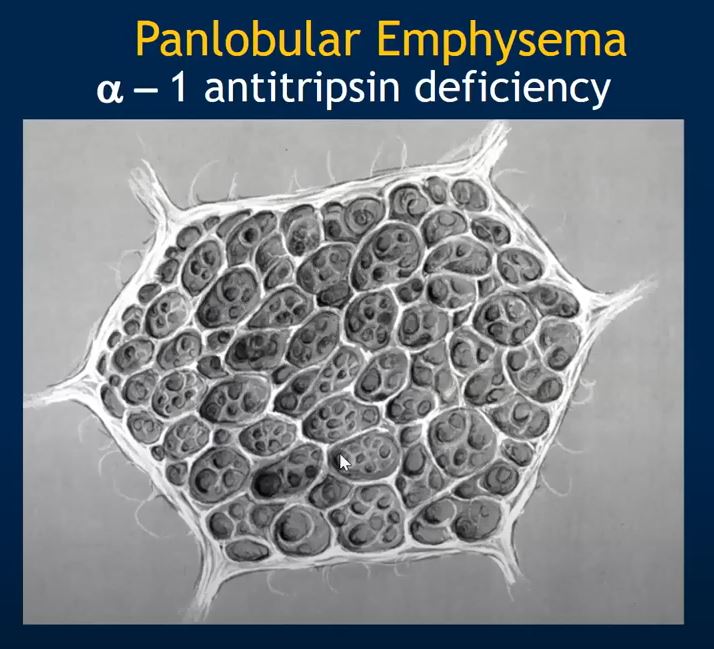
There is diffuse destruction of lung tissue throughout the secondary lobules without any evidence of localization around centrally located bronchovascular bundles as seen in centrilobular emphysema. Smoking appears to potentiate the development of panlobular emphysema in individuals with alpha-1 antitrypsin deficiency.
Courtesy YAle Rosen MD
There is diffuse destruction of lung tissue throughout the lobule as opposed to centrilobular emphysema in which the lung destruction is bronchocentric in the center of the lobule.Smoking appears to potentiate the development of panlobular emphysema in individuals with alpha-1 antitrypsin deficiency.
Courtesy Yale Rosen MD
Other Types of Emphysema
Bullous Emphysema.
large subpleural blebs or bullae (spaces >1 cm in diameter in the distended state)
= to of the four forms of emphysema, are most often subpleural, and occur near the apex, sometimes in relation to old tuberculous scarring. On occasion, rupture of the bullae may give rise to pneumothorax.
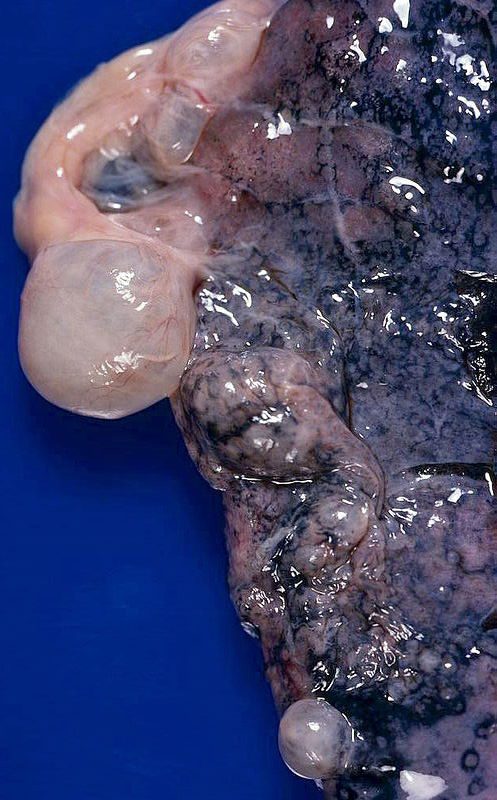
Emphysema – bullous,-subpleural_
Large, prominent subpleural bullae. Spontaneous pneumothorax often results from rupture of such lesions.
Bullous (paraseptal) emphysema limited to lung periphery. Usually not smoking-related. Rupture is most common cause of spontaneous penumothorax…mostly young adults.
Courtesy Yale Rosen MD


Large, prominent subpleural bullae. Spontaneous pneumothorax often results from rupture of such lesions.
Ashley Davidoff MD



magnified
Large, prominent subpleural bullae. Spontaneous pneumothorax often results from rupture of such lesions.
Ashley Davidoff MD
Compensatory Emphysema (Compensatory Hyperinflation).
Dilation of alveoli but not destruction of septal walls in response to loss of lung substance elsewhere. It is best exemplified by the hyperexpansion of the residual lung parenchyma


Ashley Davidoff MD


Ashley Davidoff MD
Senile Emphysema.
sometimes voluminous lungs found in the aged. These changes result from age-related alterations of the internal geometry of the lung– larger alveolar ducts and smaller alveoli–that occur without loss of elastic tissue or destruction of lung substance.
Obstructive Overinflation.
lung expands because air is trapped within it. A common cause is subtotal obstruction by a tumor or foreign object. A classic example is congenital lobar overinflation in infants, probably resulting from hypoplasia of bronchial cartilage and sometimes associated with other congenital cardiac and lung abnormalities.
Congenital lobar emphysema
Focal emphysema – Swyer James
Interstitial Emphysema.
of air stroma of the lung, mediastinum, or subcutaneous tissue is designated interstitial emphysema. In most instances, alveolar tears in pulmonary emphysema provide the avenue of entrance of air into the stroma of the lung, but rarely a wound of the chest that allows air to be sucked in or a fractured rib that punctures the lung substance may underlie this disorder. Alveolar tears usually occur when there is a combination of coughing plus some bronchiolar obstruction, producing sharply increased pressures within the alveolar sacs. Children with whooping cough and bronchitis, patients with obstruction to the airways (by blood clots, tissue, or foreign bodies) or being artificially ventilated, and individuals who suddenly inhale irritant gases provide classic examples.
J43 Emphysema
J43.0 MacLeod’s syndrome
J43.1 Panlobular emphysema
J43.2 Centrilobular emphysema
J43.8 Other emphysema
J43.9 Emphysema, unspecified
Statistics
INCIDENCE IN THE USA
Over 2 million people in the United States have emphysema, and about 32 miillion have COPD.
COPD – % SMOKERS?
90% of all COPD patients are current or former tobacco smokers.
HOW MANY SMOKERS DEVELOP COPD?
Only 15 to 20% of smokers manifest COPD. This would suggest that additional factors in a patients makeup, and this is a probable genetic predisposition, contribute to septal wall destruction.
INCIDENCE OF ALPHA 1 ANTITRYPSIN
Worldwide, approximately 1 in 2,500 individuals has alpha-1 antitrypsin deficiency. While this disorder is found in all ethnic groups, it occurs most frequently in whites of European ancestry.
HOW MANY PATIENTS WITH ALPHA 1 ANTITRYPSIN DEVELOP EMPHYSEMA?
Patients with alpha-1-antitrypsin deficiency have about a 20-fold increased risk of developing emphysema; 80-90% of deficient individuals eventually develop this condition. Smoking makes the probability and incidence significantly higher.
BEHAVIOURAL MODIFICATION
Only 6% of smokers are successful in permanent cessation. 70 to 80% who do stop smoking return to the habit.
CAUSE OF DEATH
It is the 4th highest cause of death in the USA
AUTOPSY STATISTICS
50% combined incidence of panacinar and centriacinar emphysema at autopsy and was the direct case of death in approximately 7% of these patients. About 66% of men have the disorder and only 25% of women have the disease. The presence of senile emphysema may falsely elevate these results,
STATISTICS RELATED TO TYPES
Centrilobular emphysema constitutes greater than 95% of cases. It is therefore more common than the panacinar form.
RESERVE OF THE LUNGS
Patients become symptomatic when 1/3 of lung tissue ceases to function. This is surprising and in fact may not be true since a patient can function exteremely well with only one lung post-pneumonectomy.
Chronic obstructive pulmonary disease (COPD) is estimated to affect 32 million persons in the United States and is the fourth leading cause of death in this country. P
COPD is a common medical problem affecting an estimated 16 million Americans. Males are more frequently affected than females, and Caucasians more frequently than African Americans. There is a higher prevalence of COPD among persons with a lower socioeconomic status and in those with a history of low birth weight. COPD is the fourth leading cause of death in the United States and is the only one of the 10 leading causes of death for which mortality rates are still rising. Prevalence peaks in the seventh and eighth decades, then levels off, largely due to mortality.
Some 90% of all COPD patients are current or former tobacco smokers.
Despite the strong etiologic association between smoking and COPD, only 15 to 20% of smokers lose FEV1 at a rate fast enough to manifest COPD. Epidemiologic evidence of familial clustering of COPD cases is strong and repeated, suggesting that susceptibility to the effects of tobacco smoke has genetic determinants.
Geographical Distribution
Emphysema and COPD distribution in general follows cigarette smoking habits of the world and is most prevalant in industrialized regions of the world. The This is probably related to increase air pollution in these regions and by smoke and its by products. The incidence is highest in Eastern Asia, in countries like China. European countries United States and Canada also have a high incidence .
Population affected
In general, Caucasians are affected more frequently than African Americans.
In the US in 2001,
White (non-hispanic): 2,632,331
Black (non-hispanic): 164,628
Hispanic: 130,698
Other: 55,941
INCIDENCE OF ALPHA 1 ANTITRYPSIN
Worldwide, approximately 1 in 2,500 individuals has alpha-1 antitrypsin deficiency. While this disorder is found in all ethnic groups, it occurs most frequently in whites of European ancestry.
  The Communities at Large |
| A collage of older adults with a predominance of Caucasian males.
Courtesy Ashley DAvidoff MD. 11515c01 |
Genetics
Only 15 to 20% of smokers manifest COPD. This would suggest that additional factors in a patients makeup, and this is a probable genetic predisposition, contribute to septal wall destruction. Clustering of COPD in families, is probably related to behavioral commonalities (smoking) as well as genetic makeup.
Alpha-1 antitrypsin deficiency though is a distinct genetic abnormality that is responsible for the development of COPD. Alpha-1 antitrypsin is a protein produced in the liver. Alpha-1 antitrypsin counteracts the effect of neutrophil elastase. In its absence, neutrophil elastase is free to destroy lung tissue resulting in emphysema.
Individuals with alpha-1-antitrypsin deficiency have about a 20-fold increased risk of developing emphysema; 80-90% of deficient individuals eventually develop this condition.
INCIDENCE OF ALPHA 1 ANTITRYPSIN
Worldwide, approximately 1 in 2,500 individuals has alpha-1 antitrypsin deficiency. While this disorder is found in all ethnic groups, it occurs most frequently in whites of European ancestry, and is rare in those of Oriental and African lineage.
90% of the population have -1-antitrypsin and in 10 percent the genotype is absent. PiZZ is the most common phenotype of this 10% group, and when present results in the early development of emphysema.
TRYPSIN AND ALPHA-1 ANTITRYPSIN DEFICIENCY
Trypsin is an enzyme that is released by local immune cells (and by the pancreas to aid protein digestion) is a catalyst that helps digest the protein trypsin, which assists in destroying invading bacteria. Alpha-1-antitrypsin is present in serum, tissue fluids, and macrophages and it prevents autodigestion within the respiratory tract. It functions as a major inhibitor of proteases, particularly elastase, secreted by neutrophils during inflammation. .
The incidence and mortality rates of both chronic bronchitis and emphysema may be higher in areas where air pollution is high. Bronchitis recurrences are definitely more frequent and more severe in environments with related heavy pollution, specifically with sulfur dioxide and particulate matter.
Sex Distribution
In the US in 2001,
Male: 1,678,868
Female: 1,304,730
Males are more frequently affected than females with the most severe type occurs in men who smoke heavily.
Age Distribution
In the US in 2001,
18-44: 200,259
45-64: 1,099,638
65+: 1,683,701
Older age is a risk factor for emphysema. Lung function normally declines with age. In normal individuals, FEV1 normally peaks age 25 years and there is a 35 mL per year deterioration thereafter. In patients with emphysema, it starts to present clinically early in the fifth decade, and continues on an irreversible course, aggravated by the normal aging process. Prevalence peaks in the seventh and eighth decades.
Associated Diseases
Chronic bronchitis, emphysema, and asthma are grouped together under a single umbrella of the chronic obstructive pulmonary disorders. (COPD). Although they are structurally and pathologically very different, they often are coexistant. As such, the emphysema and chronic bronchitis are linked by their common etiological agent – cigarette smoking. Continued surveillance for cancer becomes a lifetime concern for the patient and physician.
Alpha-1 antitrypsin deficiency though is a distinct genetic abnormality that is responsible for the development of COPD. Alpha-1 antitrypsin is a protein produced in the liver. and it counteracts the effect of neutrophil elastase. In its absence, neutrophil elastase is free to destroy lung tissue resulting in emphysema.
Individuals with alpha-1-antitrypsin deficiency have about a 20-fold increased risk of developing emphysema; 80-90% of deficient individuals eventually develop this condition.
Cystic fibrosis is another inherited disorder that results in chronic infections, of the lung and bronchi, with subsequent tissue destruction and emphysematous changes.
Specific Etiological Agents
Cigarette smoking is the single identifying criminal in the development of chronic bronchitis and emphysema. The prevalence of COPD shows a dose-response relationship with the number of pack-years of tobacco utilised.
The mechanism of structural damage and dysfunction appears to have many pathways.
These include;
inhibition of respiratory epithelial ciliary motility
hypertrophy of mucus glands
inhibition of alveolar macrophages on the one hand, while producing chemotactic factors that attract neutrophils and macrophages into the alveolus on the other hand.
the neutrophils are stimulted to release elastase and the macrophages are stimulated to increase elastolytic protease activity.
inhibition of alpha 1 antitrypsin activity by oxidants in cigarette smoke and oxygen free radicals secreted by neutrophils. The alpha 1 antitrypsin has an antielastase effect, and its inhibition therefore promotes the destruction of elastic material in the alveoli.
Cigarette smoke appears to cause smooth muscle contraction by vagal stimulation, resulting in an increase in resistance. Early on, the spastic effect can be reversed if the patient stops smoking.
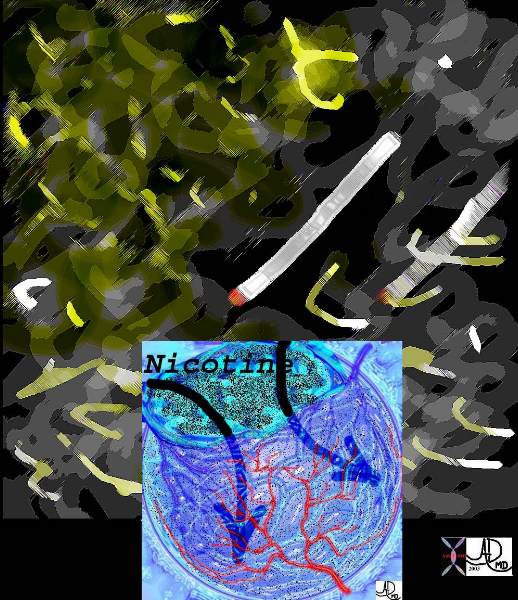 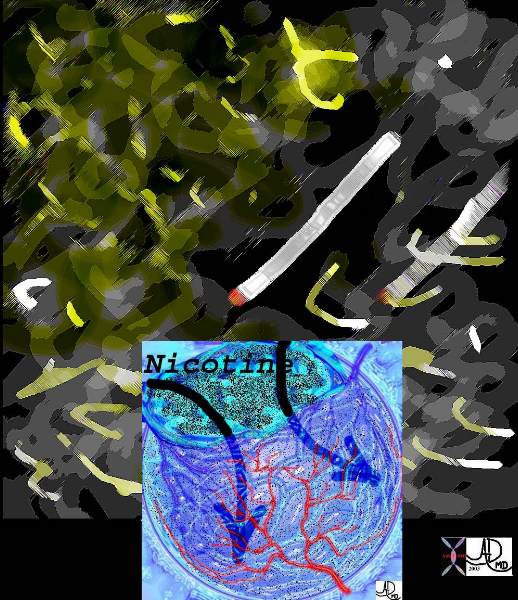 Nicotine, the Alveolus and Emphysema |
| These diseases are all about cigarettes and the garbage that they deposit in our lungs.
Courtesy Ashley Davidoff MD. 32646d |
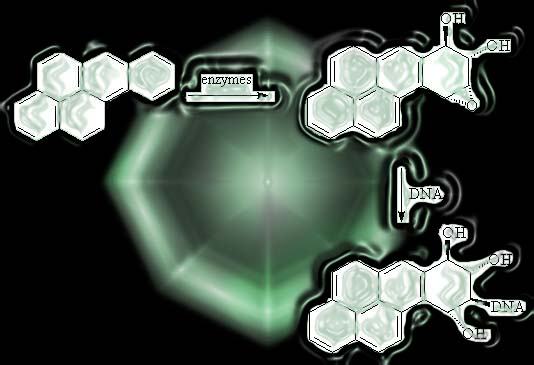 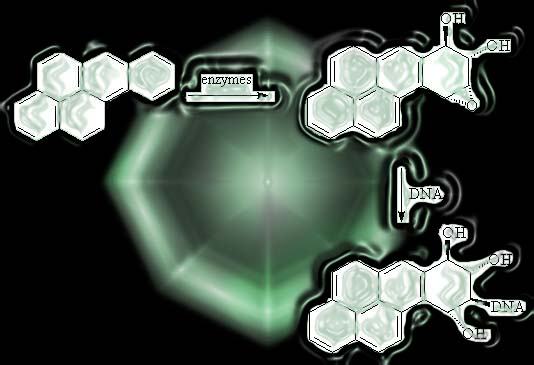 Polycyclic Aromatic Hydrocarbons |
| Polycyclic Aromatic Hydrocarbons (PAH’s) are by products of nicotine and are flat compounds that are similar to benzene in structure. Liver enzymes oxidise the PAH’s making their incorporation intpo DNA possible. The change in DNA structure leads to interference in function and a predisposition to carcinogenesis.
Image modified by Ashley Davidoff MD. 54460 |
Air Pollution
The incidence and mortality rates of both chronic bronchitis and emphysema may be higher in areas where air pollution is high. Bronchitis recurrences are definitely more frequent and more severe in environments with related heavy pollution, specifically with sulfur dioxide and particulate matter.
Pathogenesis
THE EFFECT OF SMOKE AND SMOG ON THE EPITHELIUM
Smoke and smog have similar effect on the delicate yet tenacious lining of the respiratory epithelium. In essence the pollutants cause inflammation in the airways, and by virtue of loss of mechanical defense mechanisms, and production of harmful chemical reactions, there is an acceleration of lung tissue destruction. The affliction is further aggravated by the altered physical forces and mileu in the pulmonary atmosphere. The disease is affected by the presence of associated diseases such as asthma and genetic makeup of the individual.
MECHANICAL EFFECTS
The presence of smoke in the respiratory epitheliun directly inhibits clearing mucus and secretions by temporarily disrupting the sweeping action of cilia. Permanent dysfunction and subsequent loss of the cilia with long term smoking leads to “bald” columnar cells, and progressive loss of this very imporant defnce mechanism. Increased production of mucus is also cused by smoke, and with the associated loss of ciliary function and the increased predisposition to seconadary infection by virtue of the mucus, a vicious cycle is initiated.
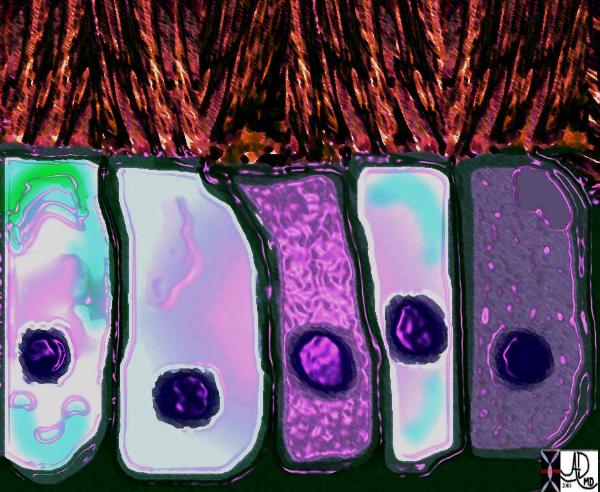  Respiratory Epithelium |
| An impression of the microscopic view of the ciliated columnar epithelium, with cilia that are sweeping dust particles to their freedom in the atmosphere.
Courtesy Ashley Davidoff MD. 70043cD08 |
  Ciliated Columnar Epithelium |
| Ciliated columnar epithelial cell, bronchial brush, right lower lobe of lung.
Courtesy tumorboard.com 54421 |
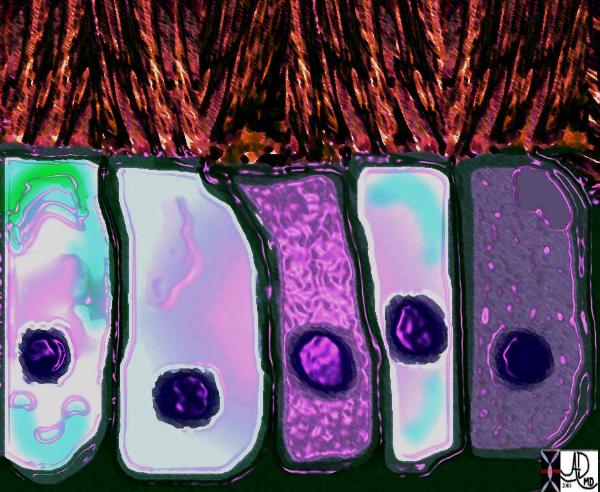
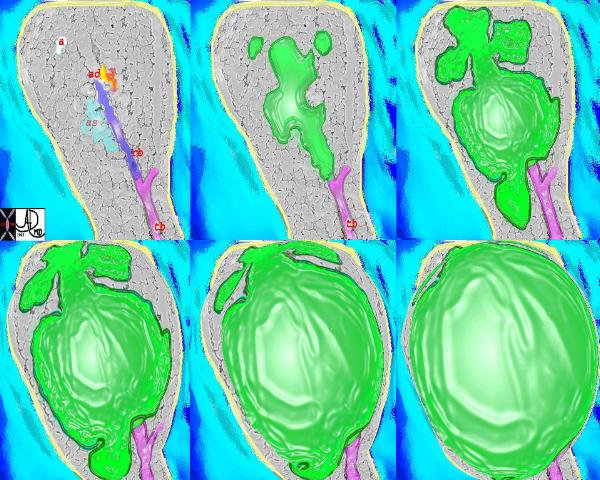 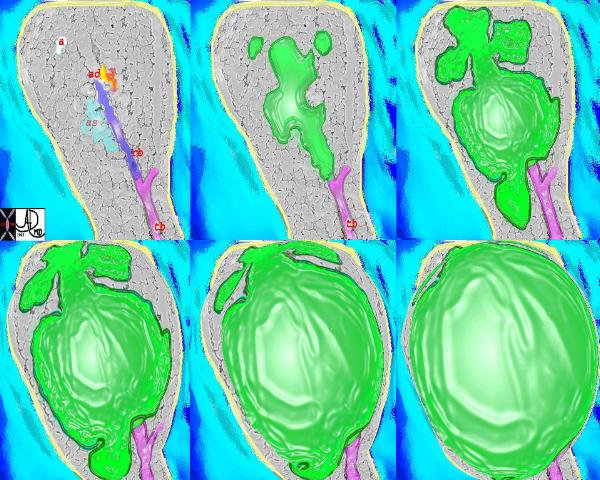 Pathogenetic Changes in Emphysema |
| An impression of the pathogenetic changes occurring in the acinus in panlobular (panacinar), with progressive enlargement of the diseased elements (in green) and incorporation compression and distortion of the normal lung. The top left image is the normal appearance with tb = terminal bronchiole(pink), rb= respiratory bronchiole, (blue) as = alveolar sac, (teal), ad = alveolar duct, (yellow-orange) and a = alveolus. (white)
Courtesy Ashley Davidoff MD 32652u |
CHEMICAL EFFECTS OF SMOKE
Decrease immunity is created by loss of mechanical as well as local Iga immune defenses, and inhibition of alpha-1 antitrypsin activity. The situation is further aggravated by excessive mucus, and as stated above creates an environment fertile for bacterial growth and secondary infection. A vicious cycle gets sets up, and the neutrophils and macrophages that are attracted to the inflammatory site, come to the aid of the host. Elastases are released, in attempt to destroy the invading organisms. These substances would otherwise also destroy host tissue but for the presence of alpha-1 antitrypsin. Since cigarette smoking also diminishes alpha-1 antitrypsin activity the protease dominance results in autodigestion of host tissue.
At a more complex level, cigarette smoke shifts the balance of oxidative and anti-oxidative chemicals by increasing the activity of oxidants and decreasing the activity of anti-oxidants. It causes the production of oxygen free radicals including superoxide, hydrogen peroxide, and hypochlorous acid, as well as assists in the production of hydroxyl radical from O2- and H2O2 by eosinophils, neutrophils, and alveolar macrophages.
The tar produced by smoking contains nitric oxide which is metabolized to cytotoxic agents.
All these factors in the end destroy lung tissue and result in the enlargement of the airspaces beyond the terminal bronchiole, with effects on the way air flows and disruption of the fine balance of ventilation and perfusion.
Complications
The complications of emphysema are mostly the complications of progressive hypoxia, and chronic smoke irritation. The patient gets progressively short of breath and the vasoconstriction of the blood vessels leads to right heart strain which can be complicated by pulmonary hypertension and cor pulmonale. Congestive cardiac failure becomes superimposed on the progressive respiratory failure.
The risks of smoking related emphysema raises the risk of developing lung carcinoma as well.
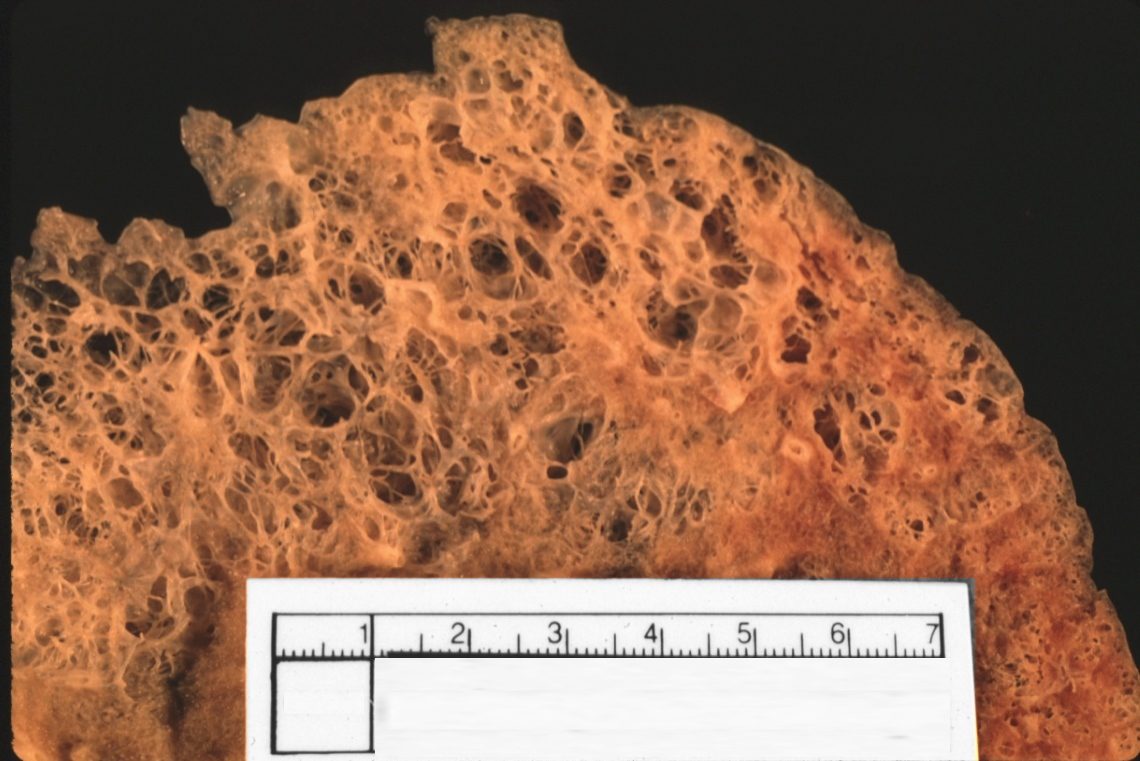
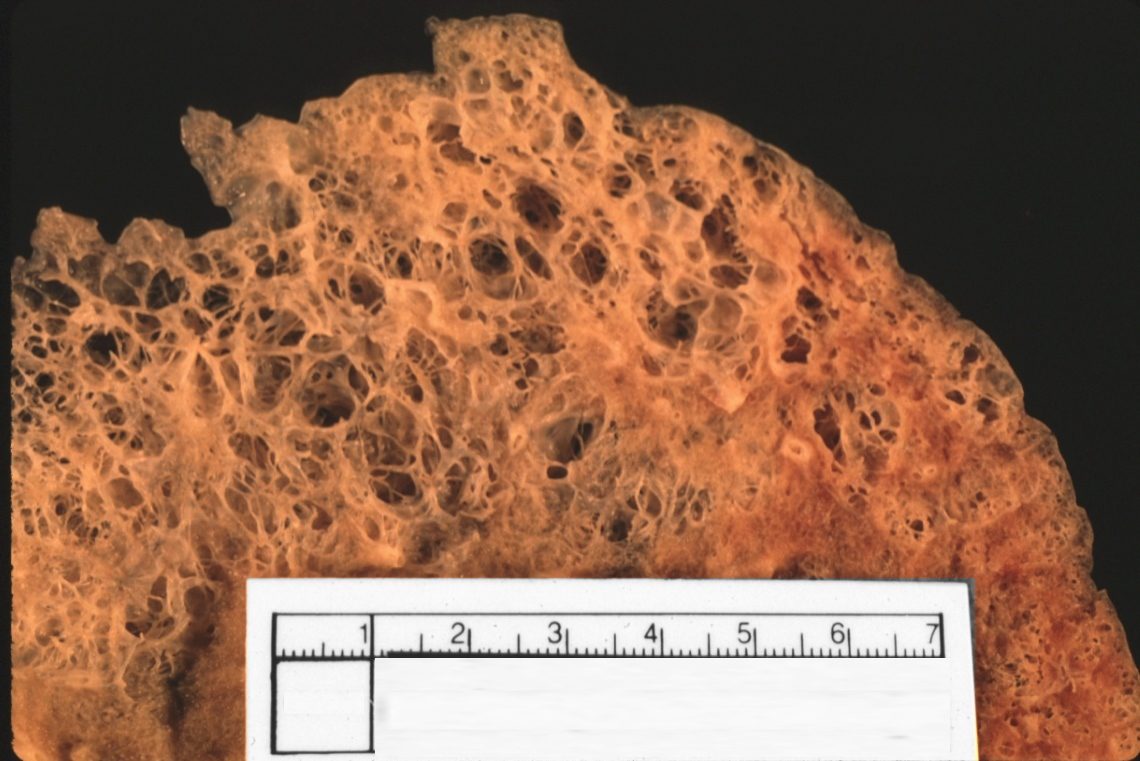
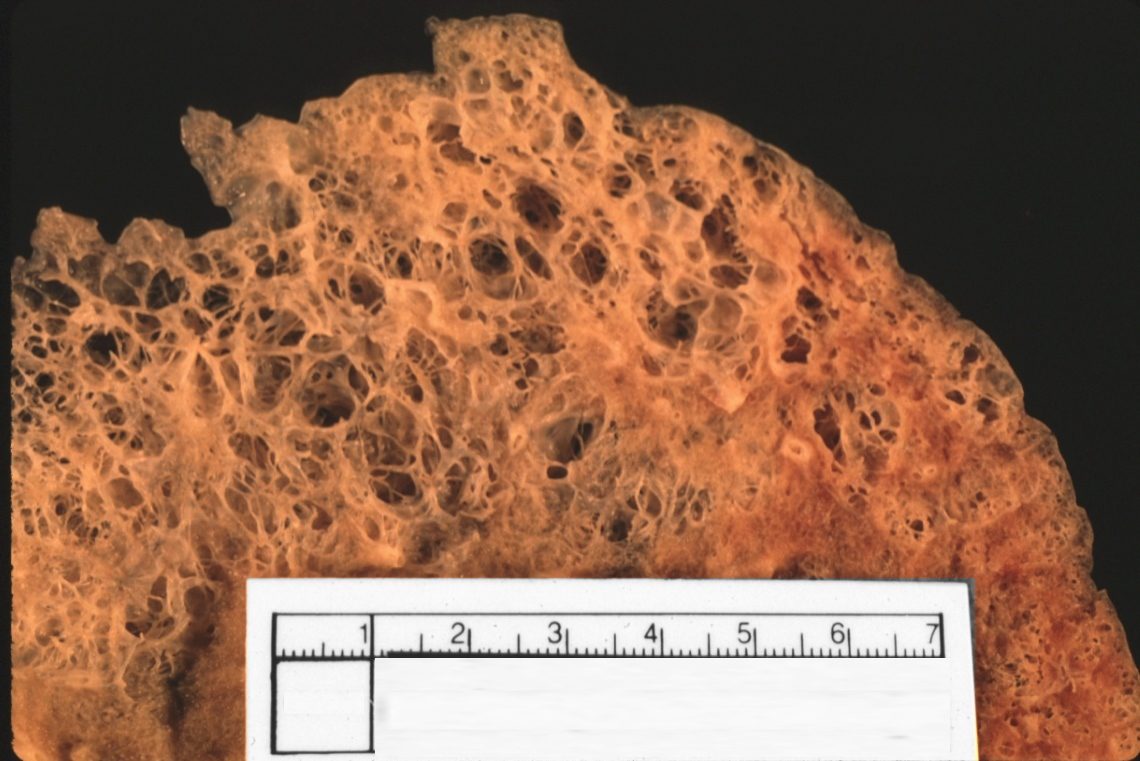
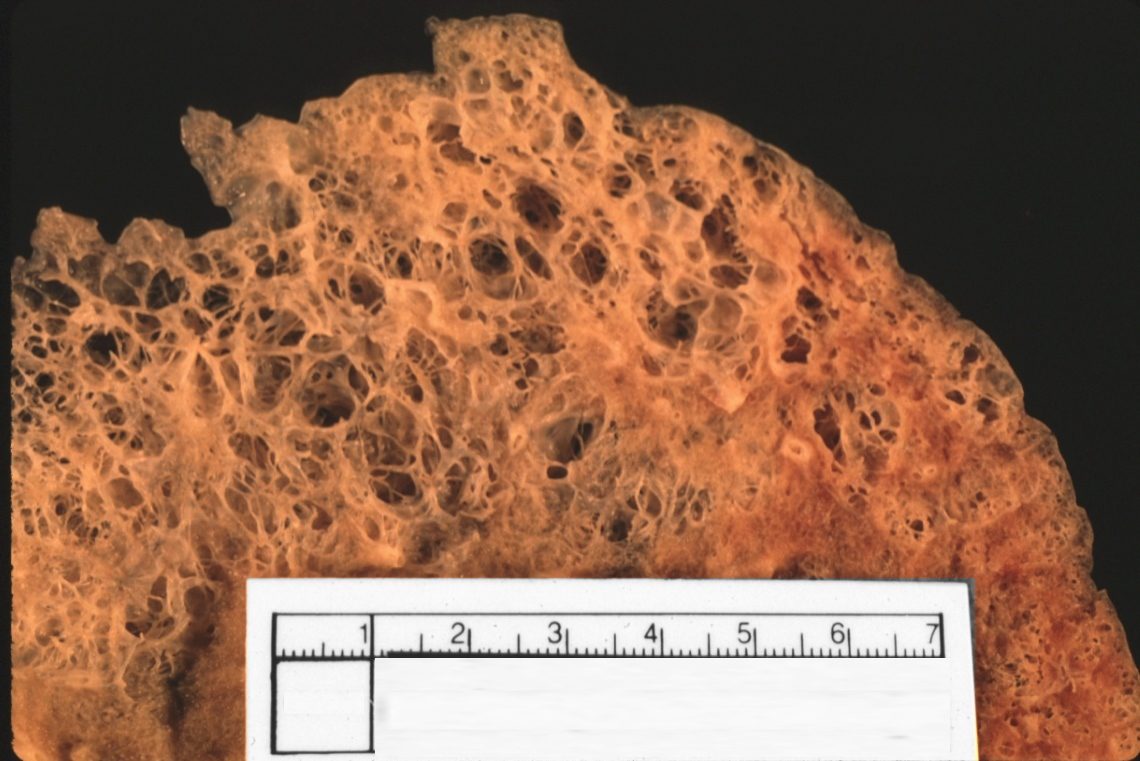
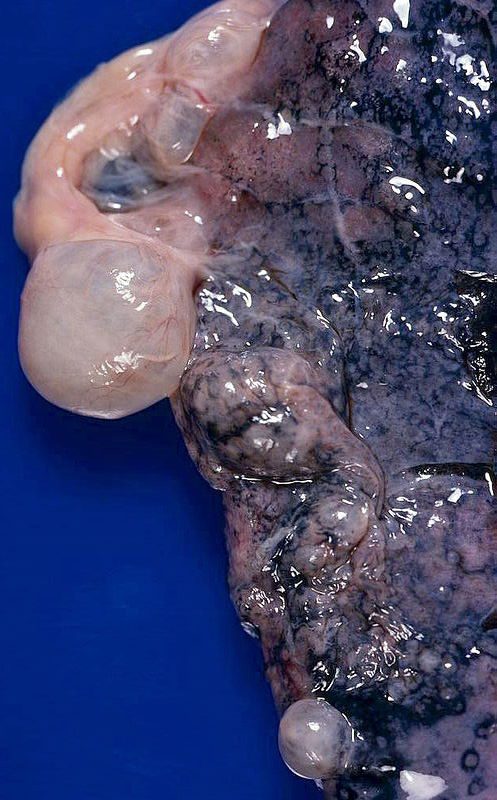
  Bulla |
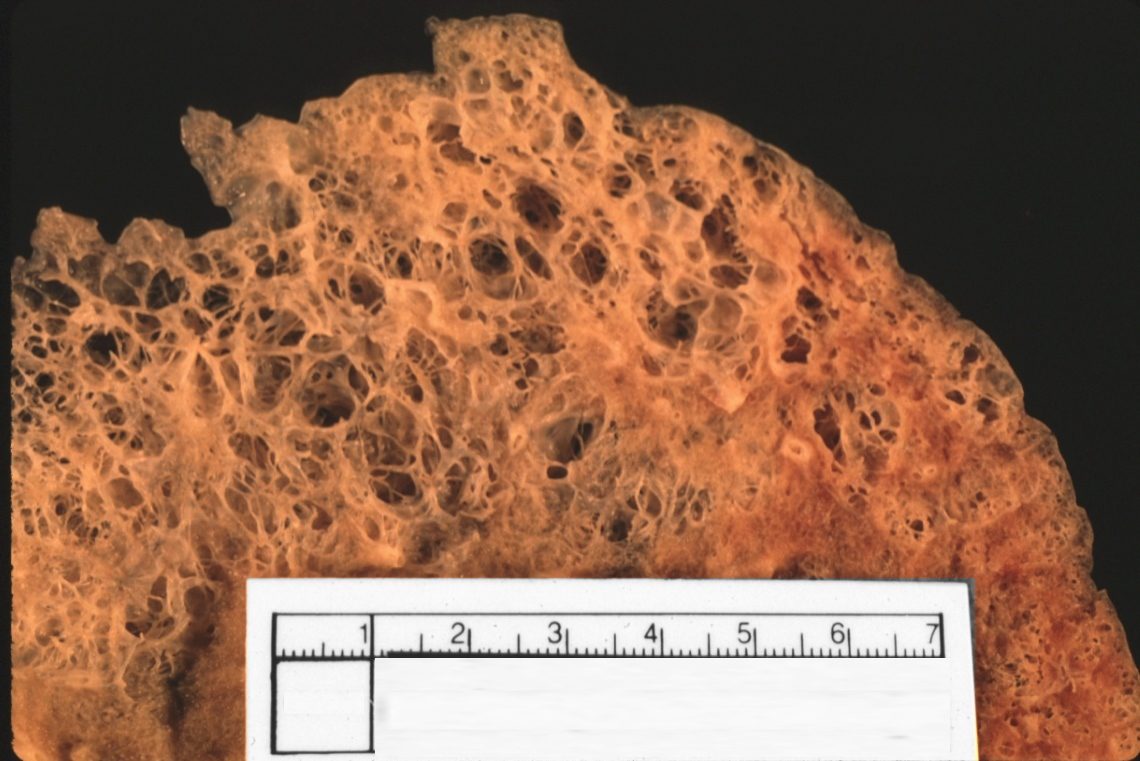
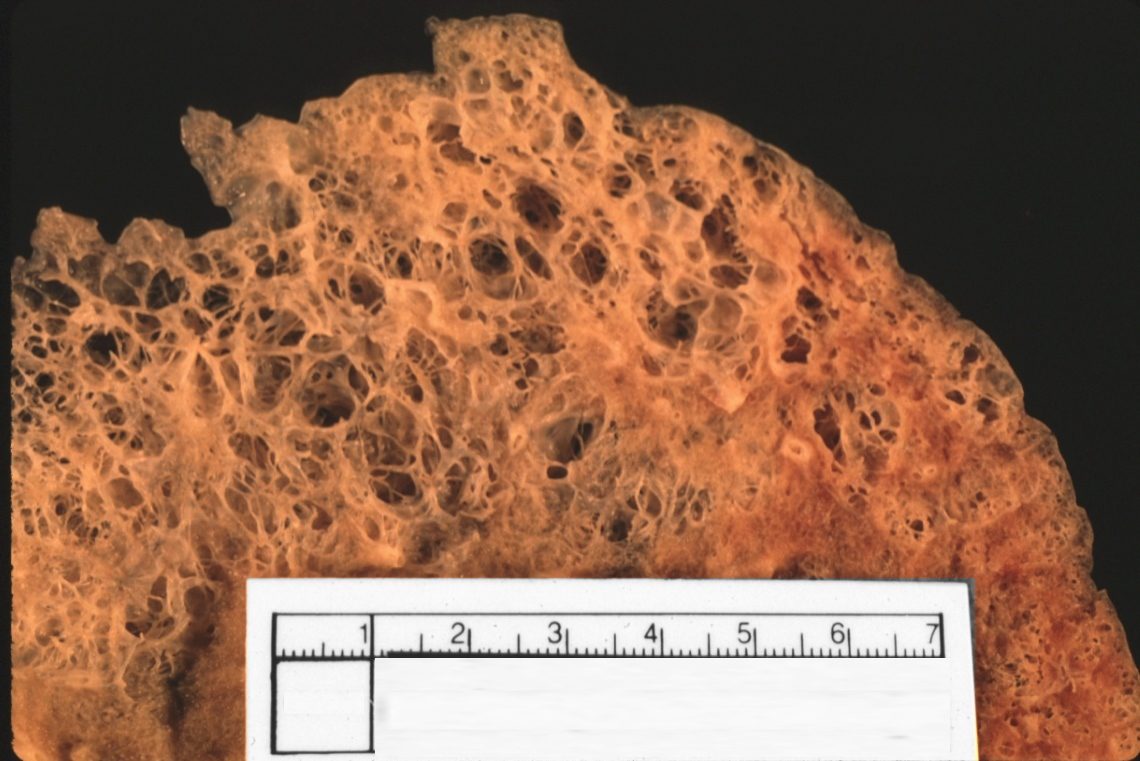
| This post mortem specimen of the apex of a left lung showing bullous lung disease caused by destruction of alveolar walls. The commonest disease association is emphysema.
Courtesy Ashley Davidoff MD. 32235 |
Natural History
The natural history of COPD evolves as a slowly progressive disorder, interrupted by intermittent episodes of pulmonary infection, usually bacterial tracheobronchitis. There is on the average one such episode per year. The clinical presentation of these episodes is characterised by increased dyspnea, worsening gas exchange, productive cough, complicated by variable degrees of edema and cardiac decompensation. The accessory muscles of respiration are put to work, as the act of breathing becomes a more conscious and mechanical effort. As a result hypercapnia results and respiratory acidosis result. Although there is significant and progressive incapacity during these episodes the patients when treated return to their pr-episode FEV1.
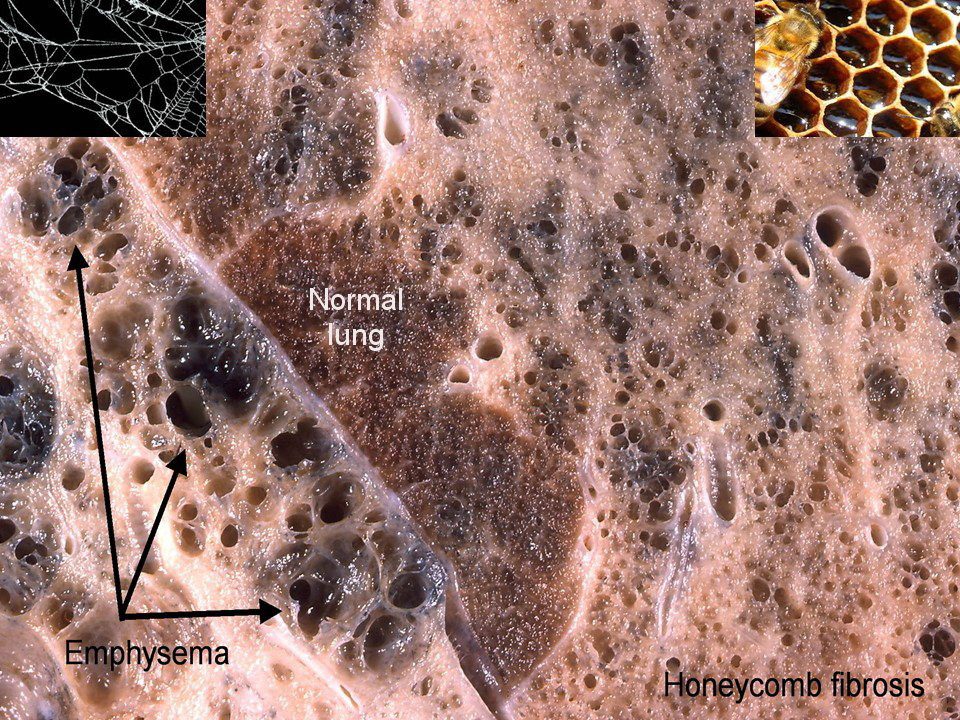
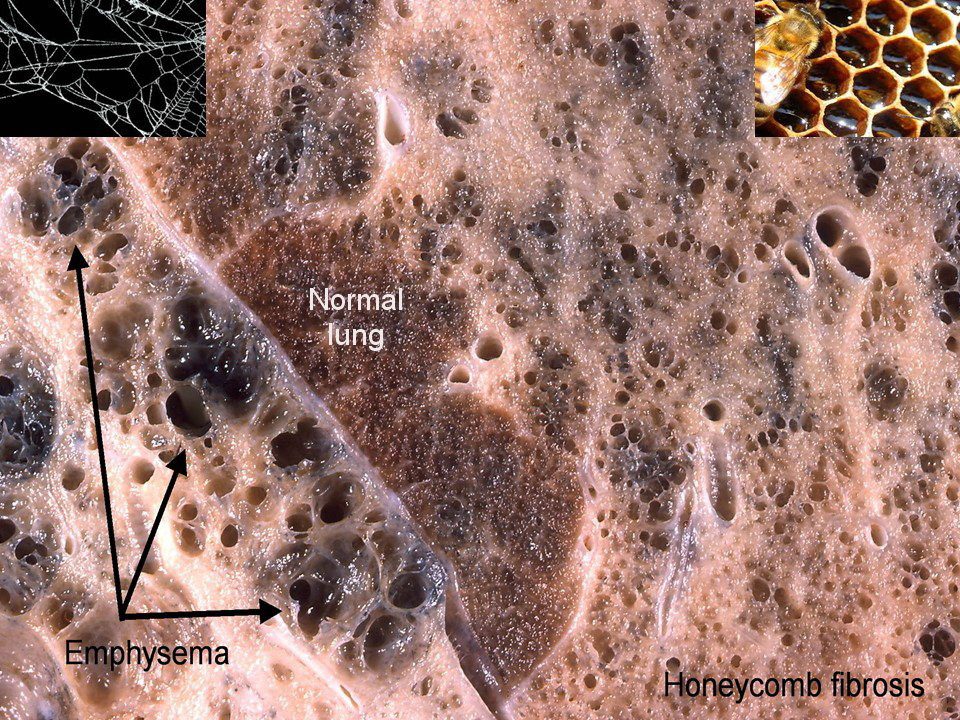
Gross Pathology
There are two major types identified, based on the macroscopic appearance (with magnifying glass). They are identified as centrilobular (centriacinar) and panlobular (panacinar). Centrilobular emphysema is more common and involves the respiratory bronchiole, whereas in panlobular emphysema involves the respiratory bronchiole, alveolar duct, alveolar sac, and the alveoli.
CENTRILOBULAR (CENTRACINAR) EMPHYSEMA
The lungs in the early stages of centrilobular emphysema, are not as impressive as the panlobular type and can look relatively normal until close magnification evaluation is made.
The alveoli in the lobule are relatively spared and so within a given lobule there are both normal and abnormal elements.
SIZE – While in mild cases the lungs may be only mildly enlarged, as the disease progresses they do become more voluminous. Again panlobular is far more impressive in size change than centrilobular disease. The emphysematous spaces are usually between .5cms- 2cms.
POSITION The disease is more common in the upper lobes and particularly involves the apical segments, and areas where fibrosis is prominent.
CHARACTER – The air spaces usually contain the pigments of the smoke and smog environment reflecting the environment of the individual.
Associated findings include the presence of inflammatory changes around the bronchi.
PANLOBULAR (PANACINAR) EMPHYSEMA
The gross pathological changes are far more impressive with panlobular emphysema, SIZE The lungs are significantly enlarged, and take over as much space of the chest cavity possible, covering the heart.
POSITION The lower lung field are more commonly involved with panlobular emphysema, and the anterior segments seem to be affected. In patients with alpha1 – antitrypsin panlobular emphysema is more common
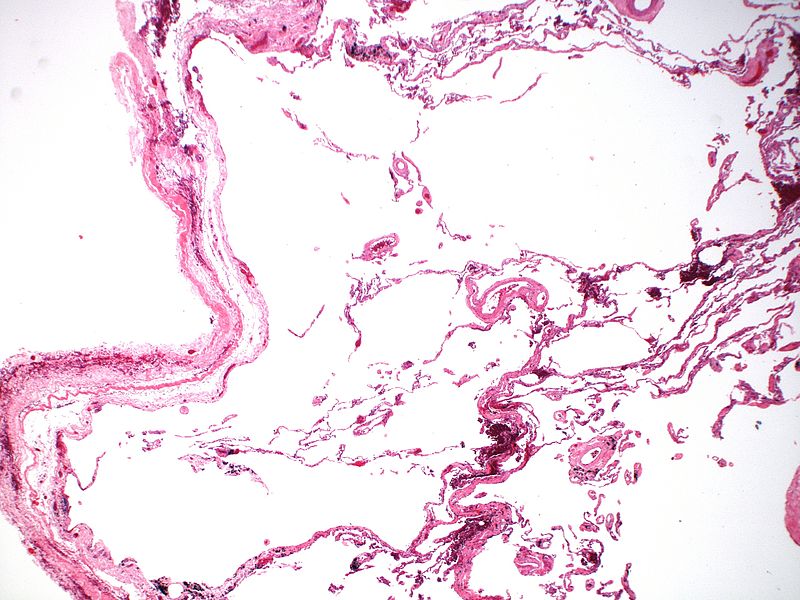
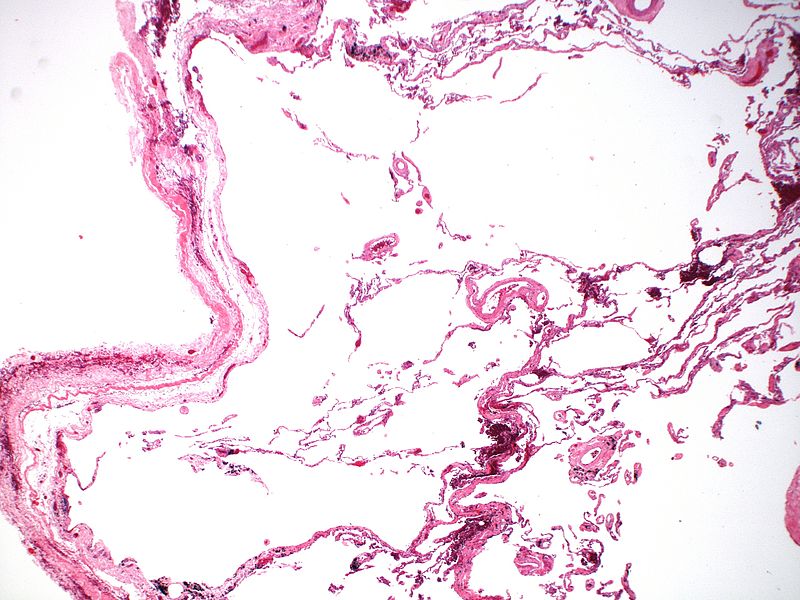
Histopathology
Microscopic examination identifies the wide open spaces together with abnormal fenestrations in the walls of the alveoli. The respiratory bronchioles and vasculature of the lung are deformed and compressed . Associated changes of bronchitis or bronchiolitis may be present.
The epithelium shows changes of chronic irritation characterised by squamous metaplasia, loss of cilia, atrophy of ciliated cells, and hypertrophy of mucus glands.
The tubular elements show variation in size, both with voluminous changes seen in the gross specimen as well as areas of narrowing caused by mucosal hyperplasia, inflammation and fibrosis.
CHARACTER The lungs appear pale because the relative lack of blood per unit of tissue – the pathological equivalent of V/Q mismatch. On closer inspection in a given lobule, no element of the lobule is spared and alveoli and respiratory bronchioles are involved.
OTHER TYPES
Paraseptal (Distal Acinar) Emphysema.
This entity has a classical appearance of dilated airspaces usually seen as a string along the pleural surfaces. Pathologically the disease is found in the upper lobes, in the distal components of the lobule, sparing the respiratory bronchiole.
Subpleural bulla has features that are similar to the paraseptal but usually is single, and may become quite large and is the source of spontaneous pneumothorax in young patients.
Chemical Factors
The carcinogenic effects of tobacco are due to the polycyclic aromatic hydrocarbons, which are found in the tars produced by combustion of tobacco. However there are innumerable (more than 1200) potentially carcinogenic substances in cigarette smoke as well as none of which have been shown to produce carcinoma in animals in the lab, but some of which have produced alveolar cell carcinoma – a carcinoma that bears the least causal relationship to smoking. Nicotine also contains carcinogens. It forms nitrosamines such as 4-(N-methyl-N-nitrosamino)-1-(3-pyridyl)-1-butanone (NNK) which was identified in tobacco smoke by Hoffmann and Hecht.
The mechanism of structural damage and dysfunction appears to have many chemically related pathways.
These include;
inhibition of alveolar macrophages on the one hand, while producing chemotactic factors that attract neutrophils and macrophages into the alveolus on the other hand.
the neutrophils are stimulated to release elastase and the macrophages are stimulated to increase elastolytic protease activity.
inhibition of alpha 1 antitrypsin activity by oxidants in cigarette smoke and oxygen free radicals secreted by neutrophils. The alpha 1 antitrypsin has an antielastase effect, and its inhibition therefore promotes the destruction of elastic material in the alveoli.
Cigarette smoke appears to cause smooth muscle contraction by vagal stimulation, resulting in an increase in resistance. Early on, the spastic effect can be reversed if the patient stops smoking.
Clinical Presentation
Emphysema (pink puffers)
These clinical changes require about 30% of the lung to be non functional.
History
Age 50-75
A long history of progressive dyspnea with late onset of nonproductive cough, with intermittent (usually annual) mucopurulent relapses, with a long standing history of smoking. Weight loss is common and may be excessive – due to the continued use of accessory muscles to aid respiration.
Examination
Patients may be very thin with a barrel chest, breathing usually assisted by pursed lips little cough, and may assume tripod sitting position.
Chest is hyper resonant, and wheezing may be heard; heart sounds are very distant. There is slowed forced expiration, reminiscent of the loss of elasticity of the chest.
Diagnostic Tests
LABORATORY TESTS
Lab Studies:
Electrolytes
CBC – Polycythemia
Pulse oximetry
Electrocardiogram
Arterial blood gas
Arterial blood gas (ABG) analysis enable evaluation of acuteness and severity.
PULMONARY FUNCTION TESTS
Decreased forced expiratory volume in 1 second (FEV1) with concomitant reduction in FEV1/forced vital capacity (FVC) ratio A normal FEV1 essentially excludes the diagnosis.
Poor/absent reversibility with bronchodilators
FVC normal or reduced
Normal or increased total lung capacity (TLC)
Increased residual volume (RV)
Normal or reduced diffusing capacity
Imaging
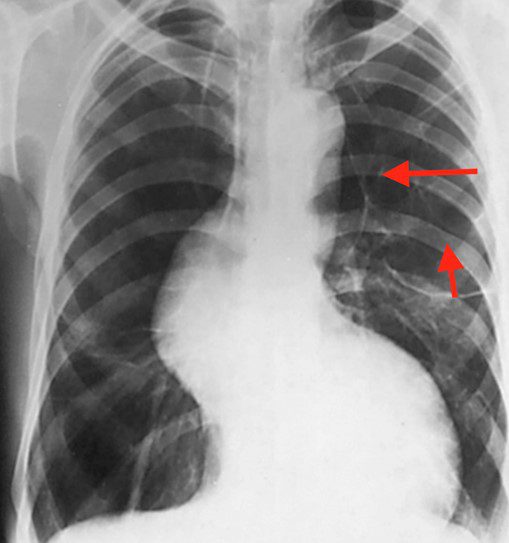
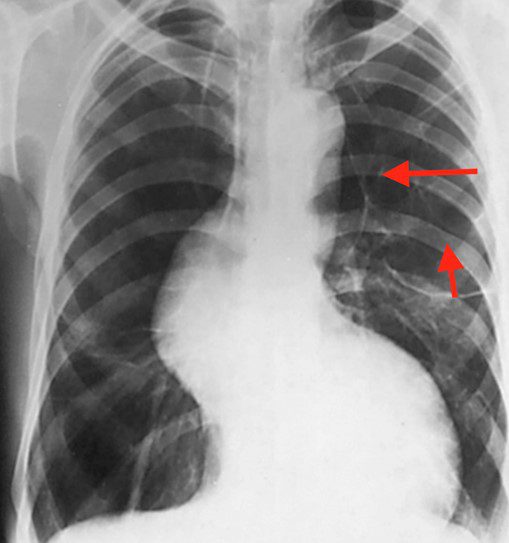
Emphysema is associated with a small heart, hyperinflation, flat hemidiaphragms, and possible bullous changes.
A P-A and lateral chest film is an useful examination and, more than any other radiological examination is helpful in evaluating lung volumes. In emphysema it may be entirely normal in mild disease. As emphysema progresses, abnormalities reflect increasing lung volumes and increasing intrathoracic pressure and pulmonary hyperinflation. The chest manifests with vertical elongation (much like an El Greco figure) with low flattened diaphragms, with similar narrowing of the heart, and increasing retrosternal air space. The clinical equivalent is the barrel shaped chest or the pectus carinatum – pigeon shaped chest. This results in an objective change of a sternal-diaphragmatic angle that exceeds 90°.
Upper lobe emphysema is the disease of smokers and is most commonly centrilobular in nature. Pan lobular disease tends to be more lower lobes characteristic of alpha1 antitrypsin deficiency.
Focal emphysematous changes are characterised by radiolucencies that are usually greater than 1 cm in diameter and surrounded by arcuate densities indicating bullous changes.
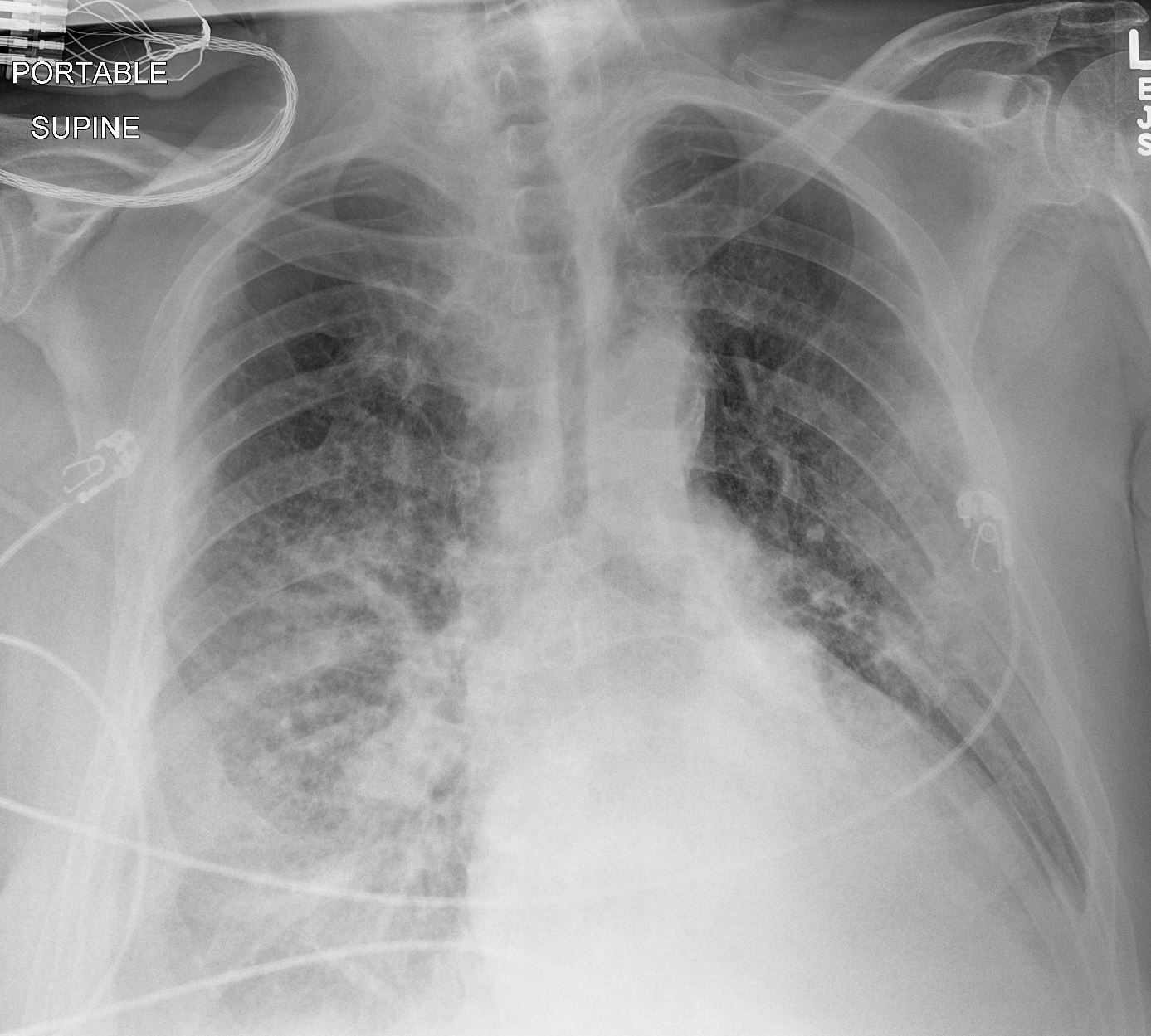
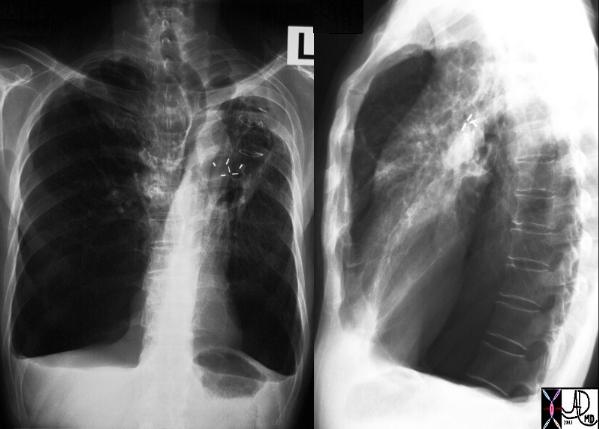 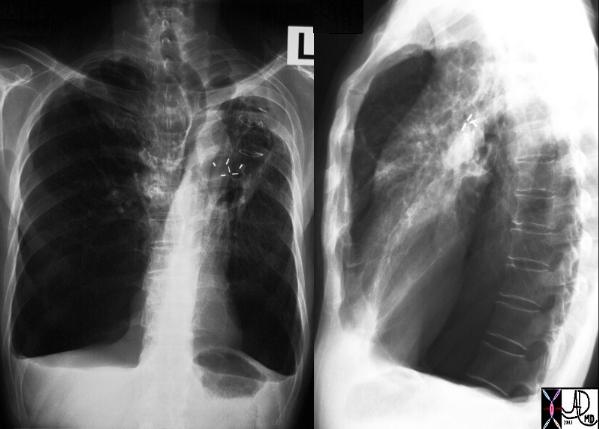 CXR Emphysema |
| A patient with hyperinflated lung volumes, COPD, and emphysema with surgical removal of a lung carcinoma from the LUL.
Courtesy Ashley Davidoff MD 30672c |
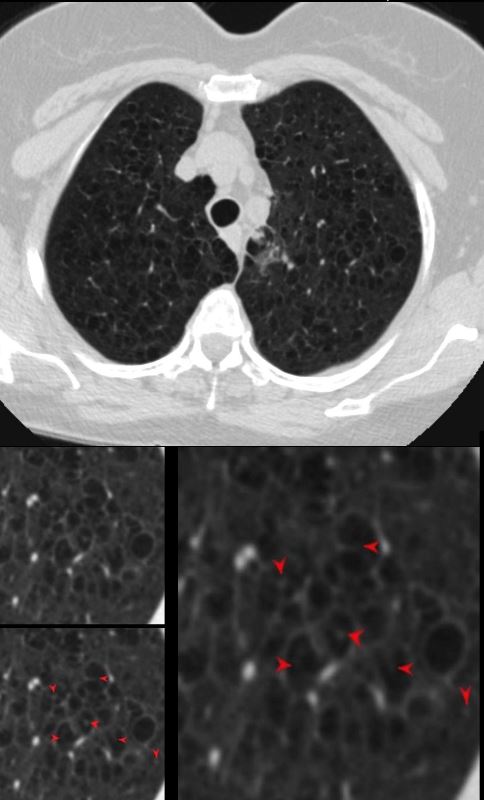
Computed tomography has greater sensitivity and specificity for emphysematous changes and particularly HRCT where mild emphysematous changes can be identified. Paraseptal emphysema and focal bulla are easily identified by CT and are relatively common. On occasion, focal emphysema caused by localized narrowing or obstruction
is well demonstrated by CT. Swyer James is such a disease caused probably by post inflammatory changes in the proximal bronchioles. Ball valve effect mechanisms operate and allow air in but not out, resulting in focal emphysema. (3030, 30316).
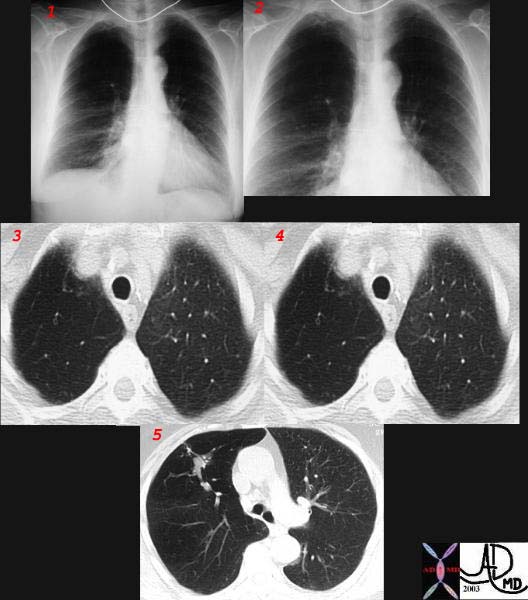 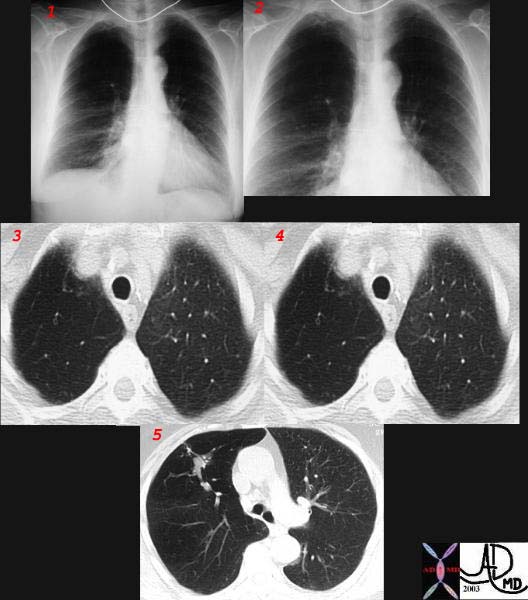 CXR and CT Emphysema |
| This combination of plain films and CT are images from a 73 year old patient with COPD. The plain films show relative lucency of the RUL compared to the LUL (1,2) with compression of the markings iof the RLL. The CT reveals focal emphysema of the RUL (3,4,5) with bronchioles expanded under pressure (3,4)and a tubular filling defect representing a large mucucs plug. A ball valve effect of this mucus plug is inferred to explain the focal emphysema that progressed over period of three months.
Courtesy Ashley Davidoff MD. 32008c |
Images courtesy of of: Crapo JD, Glassroth J, Karlinsky JB, King TE. Baum’s Textbook of Pulmonary Diseases, 7th ed, Lippincott Williams & Wilkins, Philadelphia 2004. Copyright © 2004 Lippincott Williams & Wilkins.
The distinction between centrilobular and panlobular emphysema can be made by HRCT. Usually when a segment of lung has both normal and emphysematous components, and the changes surround the accompanying artery, centrilobular emphysema is present. (32170). When the interlobular septa are seen, and this occurs more commonly in the apices, if septal destruction and thus emphysema is present then the diagnosis can be made. Even the earliest changes of small focal hyperlucent regions enable the diagnosis to be made. However it is well-known that structural changes identified on the CT may not correlate with the physiological changes and clinical presentation. Small changes may be associated with significant functional change and similarly large changes can have a minor clinical correlate.
Treatment
Elimination of tobacco smoking is the first and most significant step in the management of lung diseases associated with cigarettes. There is significant improvement in survival statistics. A significant improvement in FEV1 in the first year after smoking occurs, possibly by reversing the vasospastic changes of the often accompanying bronchitic component. Bronchodilators also help improve the FEV1 but to lesser degree.
Pulmonary rehabilitation is an important aspect of management nd requires tailoring the patients needs including physical and social aspects. Exercise disciplines, education, and behavioral intervention, are aspects that need to be addressed.
Lung Reduction surgery is an important innovation in emphysema management and is currently indicated in patients with stage III emphysema. The principles are the resection of redundant non functioning dilated lung, to provide space for the more functional lung. Early results show between 25-50% of patients benefit from the procedure.
Prognosis
The natural history of COPD evolves as a slowly progressive disorder, interrupted by intermittent episodes of pulmonary infection, usually bacterial tracheobronchitis. There is on the average one such episode per year. The clinical presentation of these episodes is characterised by increased dyspnea, worsening gas exchange, productive cough, complicated by variable degrees of edema and cardiac decompensation. The accessory muscles of respiration are put to work, as the act of breathing becomes a more conscious and mechanical effort. As a result hypercapnia results and respiratory acidosis result. Although there is significant and progressive incapacity during these episodes the patients when treated return to their pr-episode FEV1.
Emphysema is a structural disorder, and although there can be some alteration clinically with bronchodilators, the structural changes are irreversible and slowly progressive. As age advances, the emphysema progresses since loss of elasticity is part of the aging process as well. Many patients progress to respiratory and cardiac failure.


TCV – Lung Disease and Cigarette Smoking
References and Links for Emphysema
Takahashi M et al Imaging of pulmonary emphysema: A pictorial review International Journal of COPD 2008:3(2) 193–204
References and Links Smoking Related Lung Disease
Attili, A.K etal Smoking-related Interstitial Lung Disease: Radiologic-Clinical-Pathologic Correlation RadioGraphics Vol. 28, No. 5
Gupta et al Diffuse Cystic Lung Disease: Part I American Journal of Respiratory and Critical Care Medicine 191(12) April 2015
-
Videos
