
Source
Signs in Thoracic Imaging
Journal of Thoracic Imaging 21(1):76-90, March 2006.
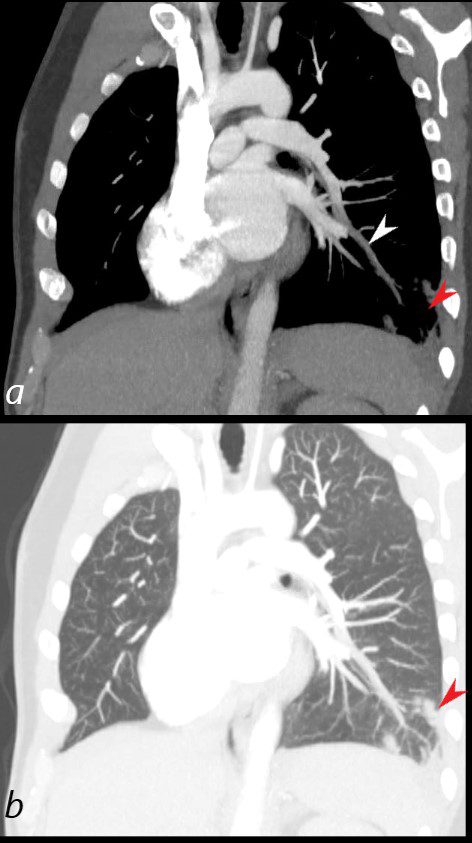
40 year old male with SLE presented with chest pain and dyspnea and initial CXR showed a vague retrocardiac density
A CT scan reconstructed in the oblique projection shows occlusive pulmonary emboli to the left lower lobe (white arrowhead,a) associated with a wedge shaped infarct (red arrowhead a,b)
Ashley Davidoff MD
key words
CT scan
SLE
PE
pulmonary embolism
pulmonary infarct

40 year old male with SLE presented with chest pain and dyspnea and initial CXR showed a vague retrocardiac density
A CT scan that followed showed occlusive pulmonary emboli to the left lower lobe (circled in white) associated with a wedge shaped infarct (red arrowhead)
Ashley Davidoff MD
key words
CT scan
SLE
PE
pulmonary embolism
pulmonary infarct
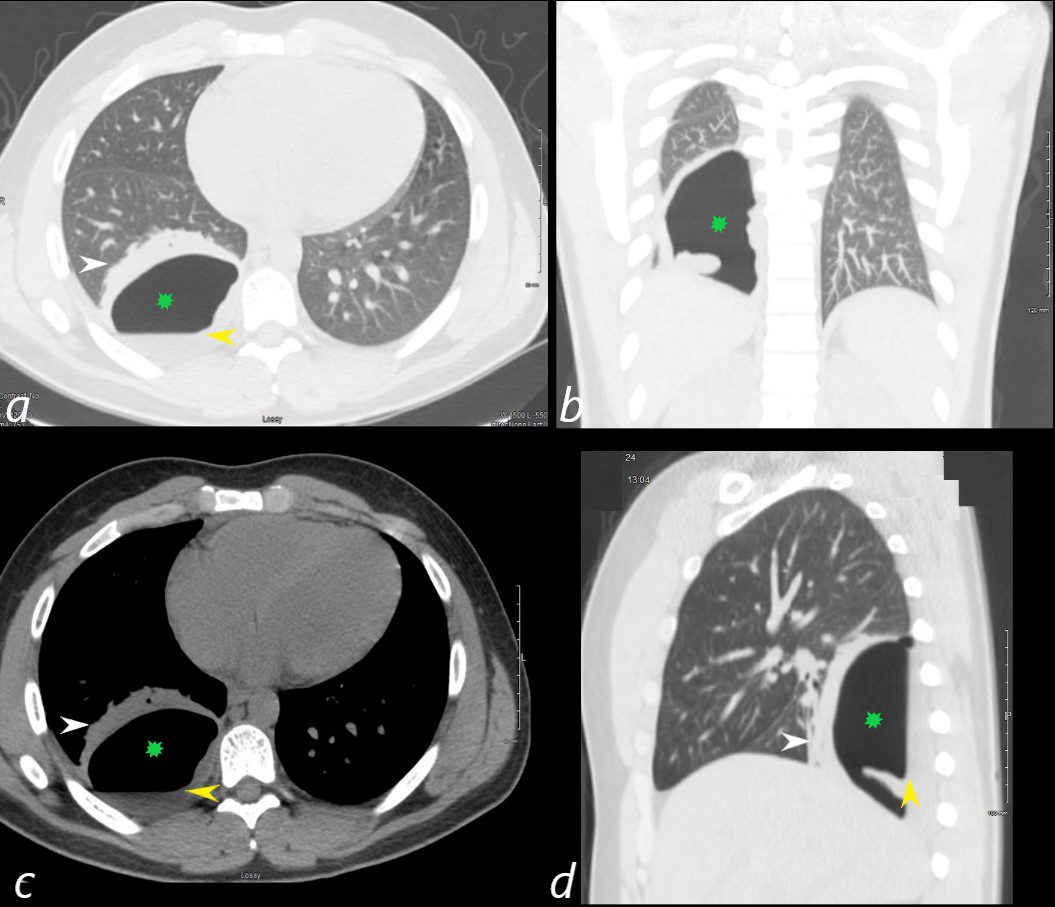
24 year old male with SLE presented with chest pain and dyspnea and initial CT showed occlusive pulmonary emboli to the right lower lobe initially associated with a wedge shaped ground glass region. 2 weeks later this evolved into a bronchopleural fistula, with a loculated pneumothorax in the right lower lobe (green star in a,b,c,d).with an air fluid level (yellow arrowhead in a,c,d) and a region of compressive atelectasis (white arrowhead a,c,d).
Ashley Davidoff MD
24 year old male with SLE presented with chest pain and dyspnea and initial CT showed occlusive pulmonary emboli to the right lower lobe (a,b, red arrowhead) with total occlusion of the right lobe artery extending into posterior basal segmental vessels (red ring d compared with normal vessels surrounded by white rin (d). An associated wedge shaped ground glass region is noted (e,f red arrowhead) representing either hemorrhage or early infarction
Ashley Davidoff MD
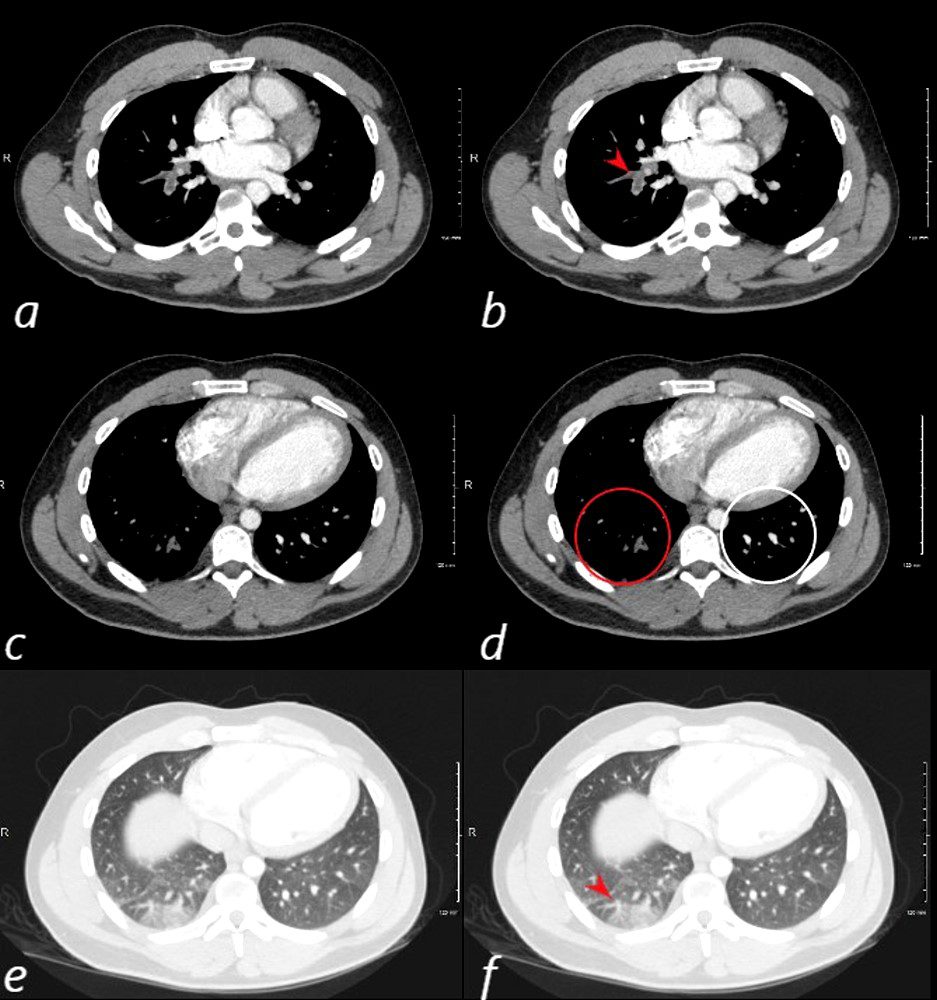
81-year-old male with weight loss, renal failure, and hemoptysis
CT axial view (a) shows multiple peripheral wedge shaped ground glass densities subtended by distended feeding vessels (a,b,c, red arrowheads) reflecting areas of microinfarction due to vasculitis that affects both the arterioles and venules.
Priscilla Slanetz MPH MD
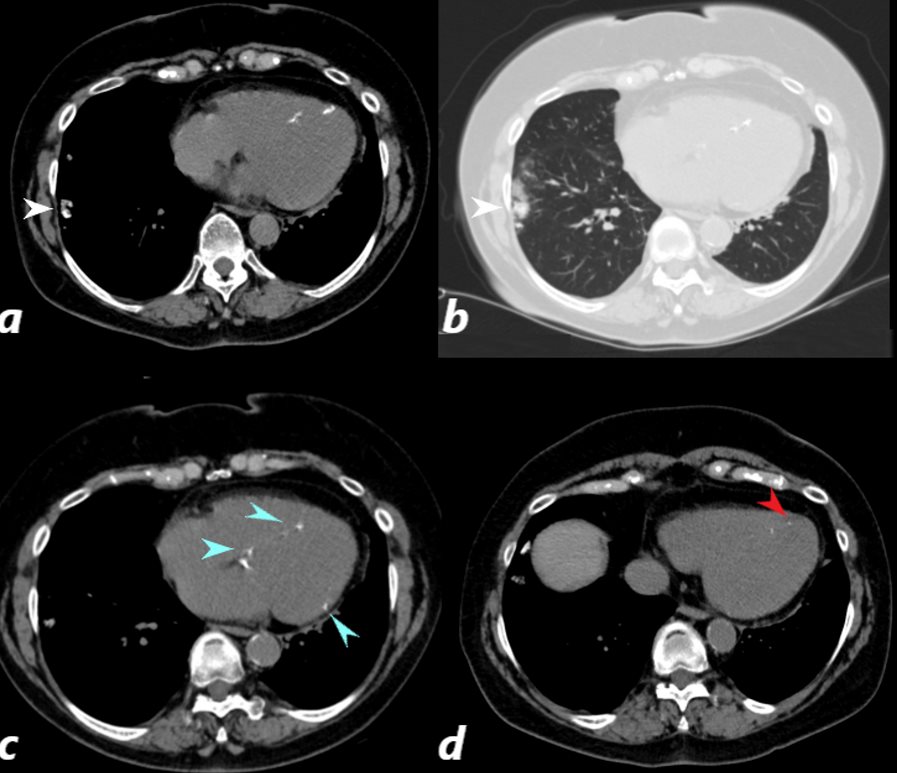
CT scan of a 67 year old female with anca vasculitis shows regions of dystrophic calcification in the lateral aspect of the right lower lobe (white arrow, a and b) )with focal nodular parenchymal consolidation, that likely reflects a site of prior small vessel infarct. Dystrophic calcification in the LV myocardium (blue arrows c) and a suggestion of fatty dysplasia in the left ventricular apex red arrow d) suggest changes from small vessel infarct. Ashley Davidoff MD

Source
Signs in Thoracic Imaging
Journal of Thoracic Imaging21(1):76-90, March 2006
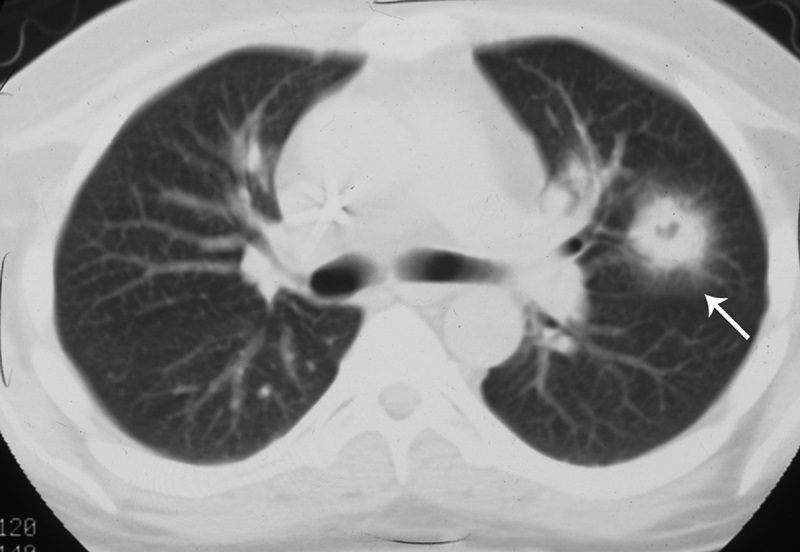
The air crescent sign appears as a variably sized, peripheral crescentic collection of air surrounding a necrotic central focus of infection on thoracic radiographs (Fig. 1A) and CT (Fig. 1B).2–4 It is often seen in neutropenic patients who have undergone bone marrow or organ transplantation and is most characteristic of infection with invasive pulmonary aspergillosis. The fungus invades the pulmonary vasculature, causing hemorrhage, thrombosis, and infarction. With time, the peripheral necrotic tissue is reabsorbed by leukocytes and air fills the space left peripherally between the devitalized central necrotic tissue and normal lung parenchyma.5 Thus, the presence of the air-crescent sign heralds recovery of granulocytic function.4 Other causes of the air crescent include cavitating neoplasms, bacterial lung abscesses, and infections such as tuberculosis or nocardiosis.6
CT halo sign
Source
Signs in Thoracic Imaging
Journal of Thoracic Imaging 21(1):76-90, March 2006.
The CT halo sign appears as a zone of ground-glass attenuation around a nodule or mass (Fig. 7) on computed tomographic (CT) images.2–4,6,28 In febrile neutropenic patients, the sign suggests angioinvasive fungal infection, which is associated with a high mortality rate in the immunocompromised host.2–4 The zone of attenuation represents alveolar hemorrhage,2,4,6,28 whereas the nodules represent areas of infarction and necrosis caused by thrombosis of small to medium sized vessels.2–4,6,28,29 Other infectious causes include candidiasis, cytomegalovirus, herpes simplex virus, and coccidioidomycosis.30 The CT halo sign may also be caused by non-infectious causes, such as Wegener granulomatosis, metastatic angiosarcoma, Kaposi sarcoma, and brochioloalveolar carcinoma (BAC).29,30 Due to the lepidic growth pattern of BAC, where the tumor cells spread along the alveolar walls, the typical ground glass halo visualized with the sign results.29
Hampton hump

Source
Signs in Thoracic Imaging
Journal of Thoracic Imaging 21(1):76-90, March 2006.
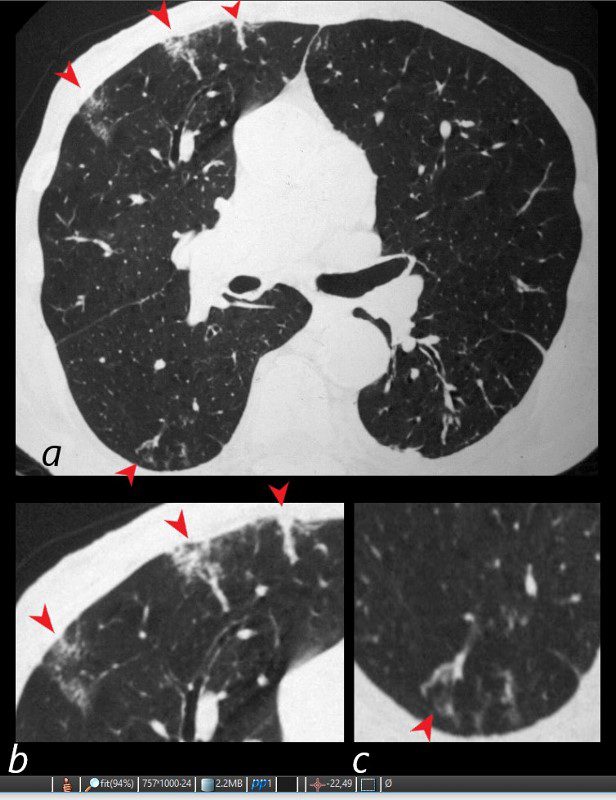
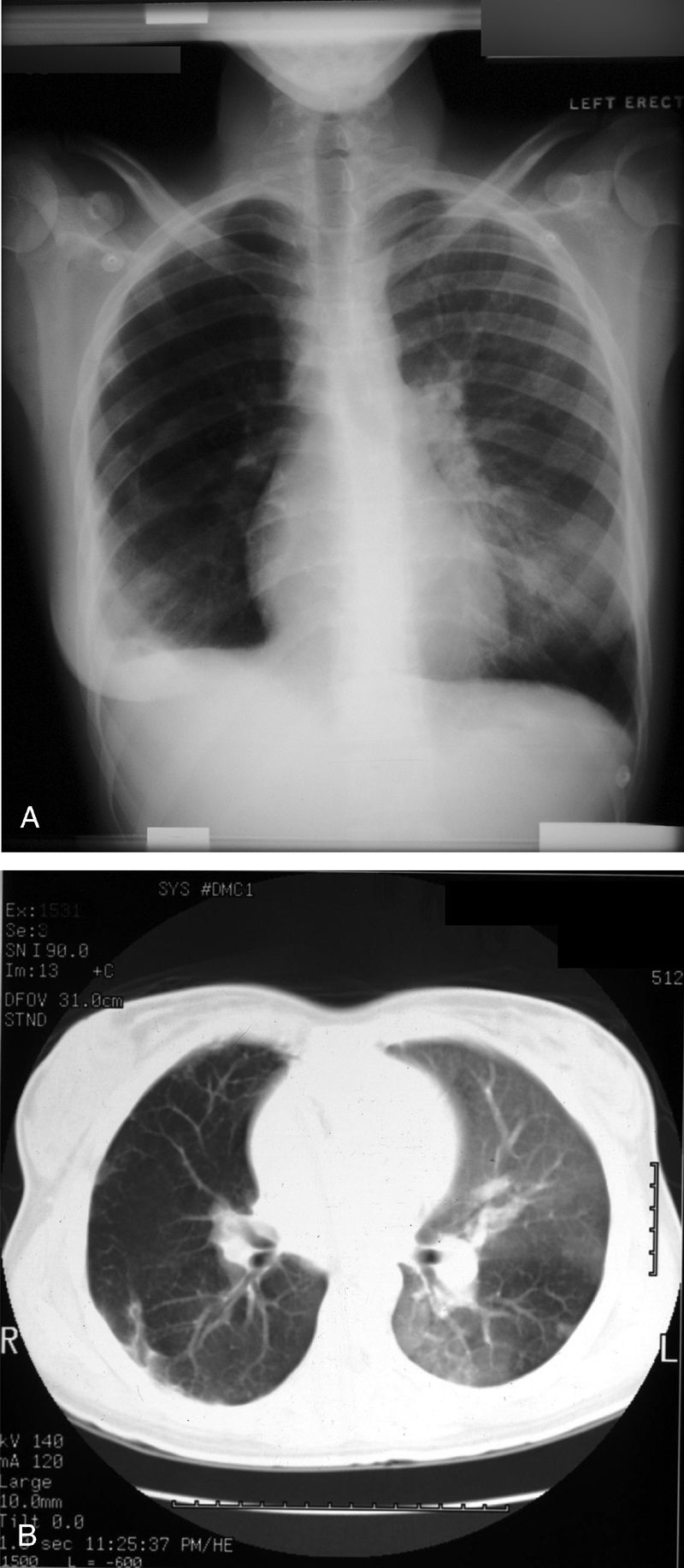
On plain radiographs (Fig. 14A) and CT (Figs. 14B, C), pulmonary infarcts are typically multifocal, peripheral in location, contiguous with one or more pleural surfaces, and more commonly confined to the lower lungs.3,47,48 The apex of these rounded or triangularly shaped opacities may point toward the hilum.3 The opacities resolve slowly over a period of several months, akin to “melting ice cubes,” and may leave a residual scar.3 The first documentation of the finding was made by Aubrey Otis Hampton, who was a practicing radiologist in the mid 1920s. He and his co-author Castleman first reported evidence of incomplete pulmonary infarction in the setting of PE in the 1940s.47,48 Autopsy follow-up showed evidence of intra-alveolar hemorrhage without alveolar wall necrosis in the first 2 days of infarction. After 2 days, wall necrosis begins and eventually leads to pulmonary infarction and an organized scar.47,48 Hampton also observed that there were differences in the healing of these incomplete infarcts depending on their premorbid cardiac history.47,48 In patients without heart disease, the incomplete infarcts would generally heal without scarring, whereas patients with congestive failure were more likely to progress to infarction with a persisting pulmonary scar.47,48 When pulmonary embolism results in infarction, airspace opacities typically develop within 12 to 24 hours.3,48
Westermark sign
Source
Signs in Thoracic Imaging
Journal of Thoracic Imaging 21(1):76-90, March 2006.
Neil Westermark was a 20th-century German radiologist who first discovered that a certain subset of patients diagnosed with pulmonary embolism (PE) were complicated by pulmonary infarction.64 He described the “anemic” or oligemic peripheral regions of lung parenchyma as “wedge-shaped shadows.” Interestingly, he also found that the majority of patients with PE did not have pulmonary infarcts, a finding that has been affirmed in the more recent literature.47 The chest radiograph (Fig. 24A) and CT (Fig. 24B) findings of increased translucency (chest radiograph) or hypoattenuation (CT) corresponding to oligemia in the periphery of the lung distal to an occlusive arterial embolus is typical.3,4,64 Visualization typically signifies either occlusion of a larger lobar or segmental artery or widespread small vessel occlusion.4,64
